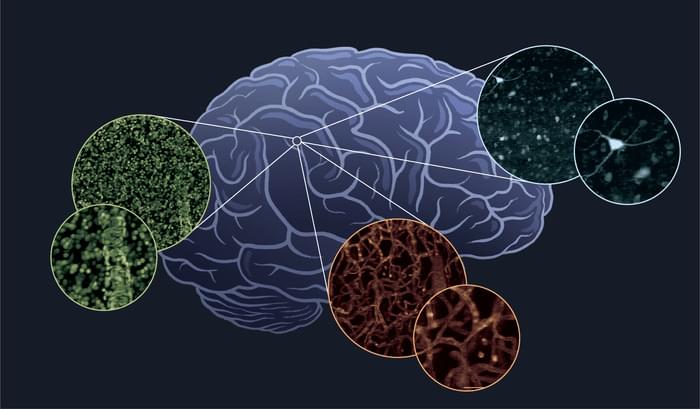
Traditionally, research showed tumor tissue to be free of microbes. In recent years, however, technology has advanced, allowing scientists to detect tiny numbers of bacteria that have taken up residence inside tumor tissue. For example, Shang Cai and his team detected 135,000 microorganisms in a gram of mouse breast tumor tissue, almost ten times more than in healthy tissue. (By comparison, a gram of feces has roughly 300 billion microbes.) Furthermore, nearly all the bacteria were living inside the mouse cells.
The biological significance of the intratumor microbiota remains largely unknown. However, scientists have found that the gut microbiota contributes to tumor progression. Cai wanted to know if these tumor-infesting intracellular bacteria are also involved in cancer progression.