The second half of Tsiolkovsky’s famous quote refers to not just living on the Earth but relying on it as we venture farther out into the cosmos. Even today, as the International Space Station orbits above at 28,000 kilometers per hour (17,500 miles per hour), those astronauts require constant resupply from the ground to stay alive. Future astronauts on the Moon might only have to wait three days to receive supplies from Earth, but as we move farther out into space, especially to Mars, this reliance will undoubtedly become far more tedious, time-consuming, and costly. Therefore, if humanity is to establish a long-term presence in space, we have to learn to use the on-hand resources we have at our disposal.
A team of researchers from the Indian Institute of Science (IISc), in collaboration with the Indian Space Research Organisation (ISRO), has developed a sustainable method for making bricks out of Martian soil, using bacteria and urea. Mammals, including humans, are the primary producers of urea. Because they secrete urea as the primary nitrogenous waste product, they are called ureotelic animals. Urea serves an important role in the metabolism of nitrogen-containing compounds by animals. These so-called “space bricks” can be used to construct building-like structures on Mars that could facilitate human settlement on the Red Planet.
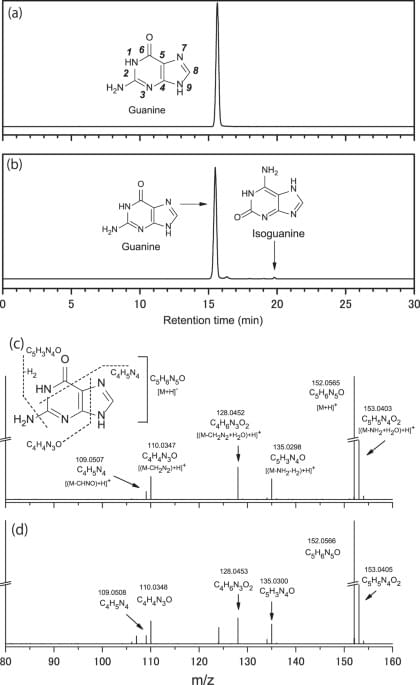
The method for making these space bricks was published in PLOS One. A slurry is first created by mixing Martian soil (simulant) with guar gum, a bacterium called Sporosarcina pasteurii, urea, and nickel chloride (NiCl2). This slurry can be poured into molds of any desired shape, and over a few days, the bacteria convert the urea into crystals of calcium carbonate. These crystals, along with biopolymers secreted by the microbes, act as the cement holding the soil particles together. An advantage of this method is the reduced porosity of the bricks, which has been a problem with other methods used to consolidate Martian soil into bricks.