Circa 2021 face_with_colon_three
A datacentre that fits in the palm of your hand? However, right now, DNA storage is an expensive chemical process that researchers are trying to make a practical proposal.

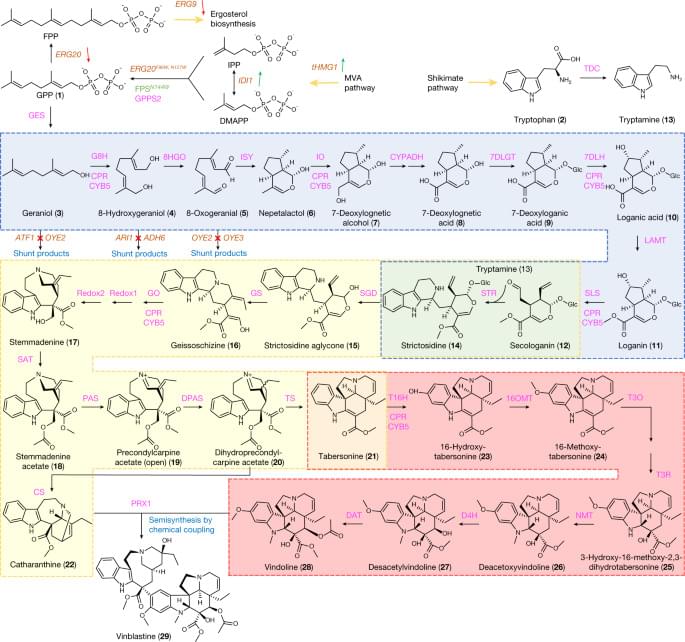
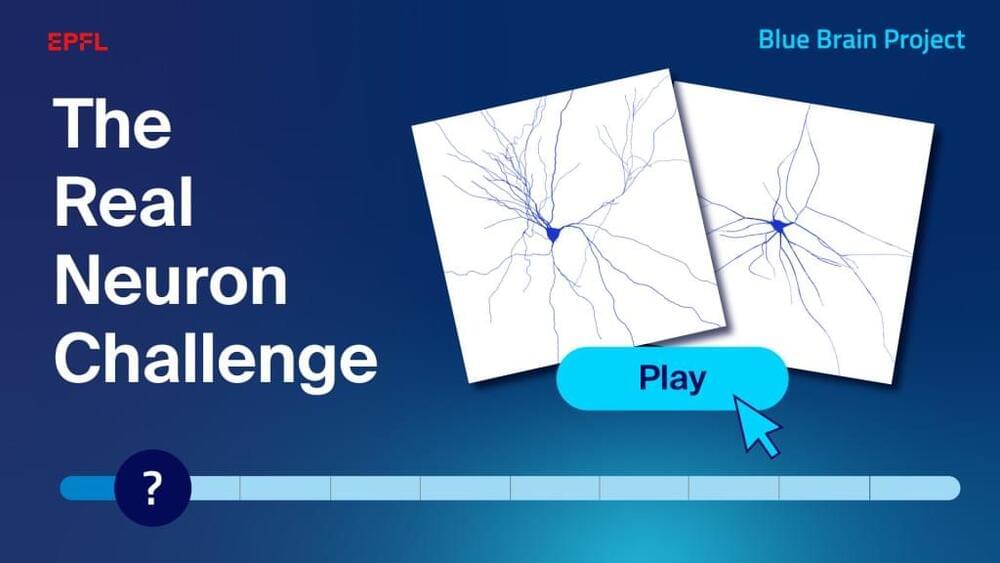
In a study published in Cell Reports, we present a novel algorithm for the digital generation of neuronal morphologies, based on the topology of their branching structure. This algorithm generates neurons that are statistically similar to the biological neurons, in terms of morphological properties, electrical responses and the connectivity of the networks they form.
This study represents a major milestone for the Blue Brain Project and for the future of computational neuroscience. The topological neuron synthesis enables the generation of millions of unique neuronal shapes from different cell types. This process will allow us to reconstruct brain regions with detailed and unique neuronal morphologies at each cell position.
The topological representation of neurons facilitates the generation of neurons that approximate morphologies that are structurally altered compared to healthy neuronal morphologies. These structural alterations of neurons are disrupting the brain systems and are contributing factors to brain diseases. The topological synthesis can be used to study the differences between healthy and diseased states of different brain regions and specifically, what structural alterations of neurons are causing important problems to the networks they form.

Scientists have discovered that increasing the production of new neurons in mice with Alzheimer’s.
Alzheimer’s disease is a disease that attacks the brain, causing a decline in mental ability that worsens over time. It is the most common form of dementia and accounts for 60 to 80 percent of dementia cases. There is no current cure for Alzheimer’s disease, but there are medications that can help ease the symptoms.

A team of University of British Columbia researchers working on developing oral insulin tablets as a replacement for daily insulin injections have made a game-changing discovery.
Researchers have discovered that insulin from the latest version of their oral tablets is absorbed by rats in the same way that injected insulin is.
“These exciting results show that we are on the right track in developing an insulin formulation that will no longer need to be injected before every meal, improving the quality of life, as well as mental health, of more than nine million Type 1 diabetics around the world.” says professor Dr. Anubhav Pratap-Singh (he/him), the principal investigator from the faculty of land and food systems.


Foresight Existential Hope Group.
Program & apply to join: https://foresight.org/existential-hope/
In the Existential Hope-podcast (https://www.existentialhope.com), we invite scientists to speak about long-termism. Each month, we drop a podcast episode where we interview a visionary scientist to discuss the science and technology that can accelerate humanity towards desirable outcomes.
Xhope Special with Foresight Fellow Morgan Levine.
Morgan Levine is a ladder-rank Assistant Professor in the Department of Pathology at the Yale School of Medicine and a member of both the Yale Combined Program in Computational Biology and Bioinformatics, and the Yale Center for Research on Aging. Her work relies on an interdisciplinary approach, integrating theories and methods from statistical genetics, computational biology, and mathematical demography to develop biomarkers of aging for humans and animal models using high-dimensional omics data. As PI or co-Investigator on multiple NIH-, Foundation-, and University-funded projects, she has extensive experience using systems-level and machine learning approaches to track epigenetic, transcriptomic, and proteomic changes with aging and incorporate.
this information to develop measures of risk stratification for major chronic diseases, such as cancer and Alzheimer’s disease. Her work also involves development of systems-level outcome measures of aging, aimed at facilitating evaluation for geroprotective interventions.
Existential Hope.
A group of aligned minds who cooperate to build beautiful futures from a high-stakes time in human civilization by catalyzing knowledge around potential paths to get there and how to plug in.
Follow us!
Twitter: https://twitter.com/HopeExistential.
Instagram: https://www.instagram.com/existential.hope/