The Tracy lab focuses on the KIBRA protein.

😗 year 2017.
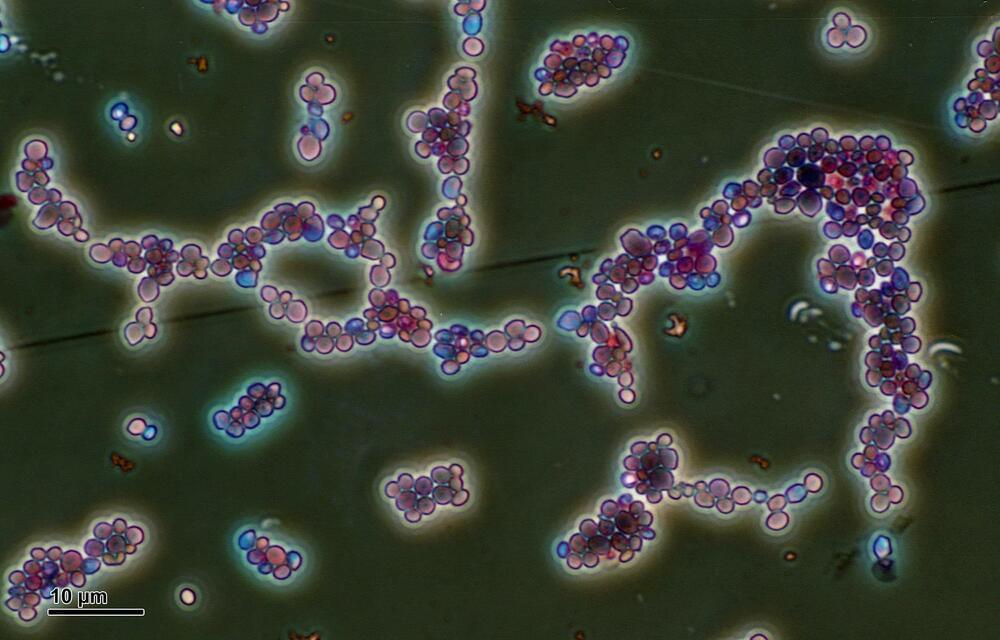
Certain treatments for patients suffering from chronic diseases, such as inflammatory bowel diseases, require multiple intravenous or subcutaneous injections of specific drugs. Because of the pain and anxiety associated with needles, some patients stop adhering to these treatments.
MIT spinout Portal Instruments has now landed a commercialization deal for a smart, needle-free injection device that could reduce the pain and anxiety associated with needle injections, shorten administration time, and improve patient adherence.
Based on years of MIT research, the startup developed a jet-injection device that delivers a rapid, high-pressure stream of medicine, as thin as a strand of hair, through the skin in adjustable dosages, causing little to no pain. A connected app tracks each dose and the medicine’s effects, and uploads that information to the cloud, for patients and doctors. The device would be sold as a drug-device combination product to medical professionals and provided to patients with a prescription.
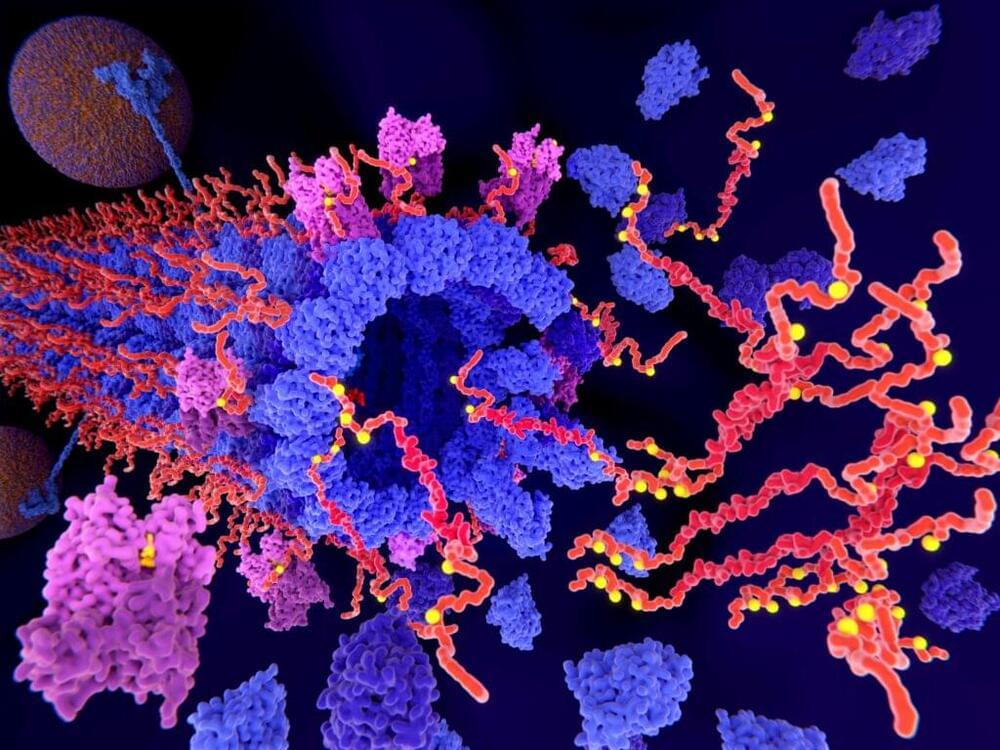
EPFL researchers have created novel protein binders that can seamlessly attach to important targets, including the spike protein of SARS-CoV-2.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the official name of the virus strain that causes coronavirus disease (COVID-19). Previous to this name being adopted, it was commonly referred to as the 2019 novel coronavirus (2019-nCoV), the Wuhan coronavirus, or the Wuhan virus.


Last week, US-Israeli startup SIRTLab announced the appointment of leading geroscience researcher Nir Barzilai as its Chief Medical Adviser. The company is focused on the development of therapeutics that boost levels of a key protein called sirtuin 6 (SIRT6), which is heavily implicated in longevity.
Sirtuins are a group of proteins found in all living organisms, including humans, that play a vital role in regulating various cellular processes. There are seven different types of sirtuins, numbered from SIRT1 to SIRT7, each with its own unique functions. In recent years, SIRT6 has gained particular attention for its potential role in promoting healthy aging, and SIRTLab has put the protein at the center of its work.
Longevity. Technology: The SIRT6 protein has been shown to regulate several critical cellular pathways, including glucose metabolism, DNA repair and inflammation – all of which play key roles in aging and longevity. One of the world’s leading authorities on SIRT6 is SIRTLab co-founder and Bar-Ilan University professor Haim Cohen, whose research is behind the company’s work to develop therapeutics with longevity-boosting potential. To learn more about SIRTLab’s longevity-first approach, we spoke to its co-founder and CEO Boaz Misholi.
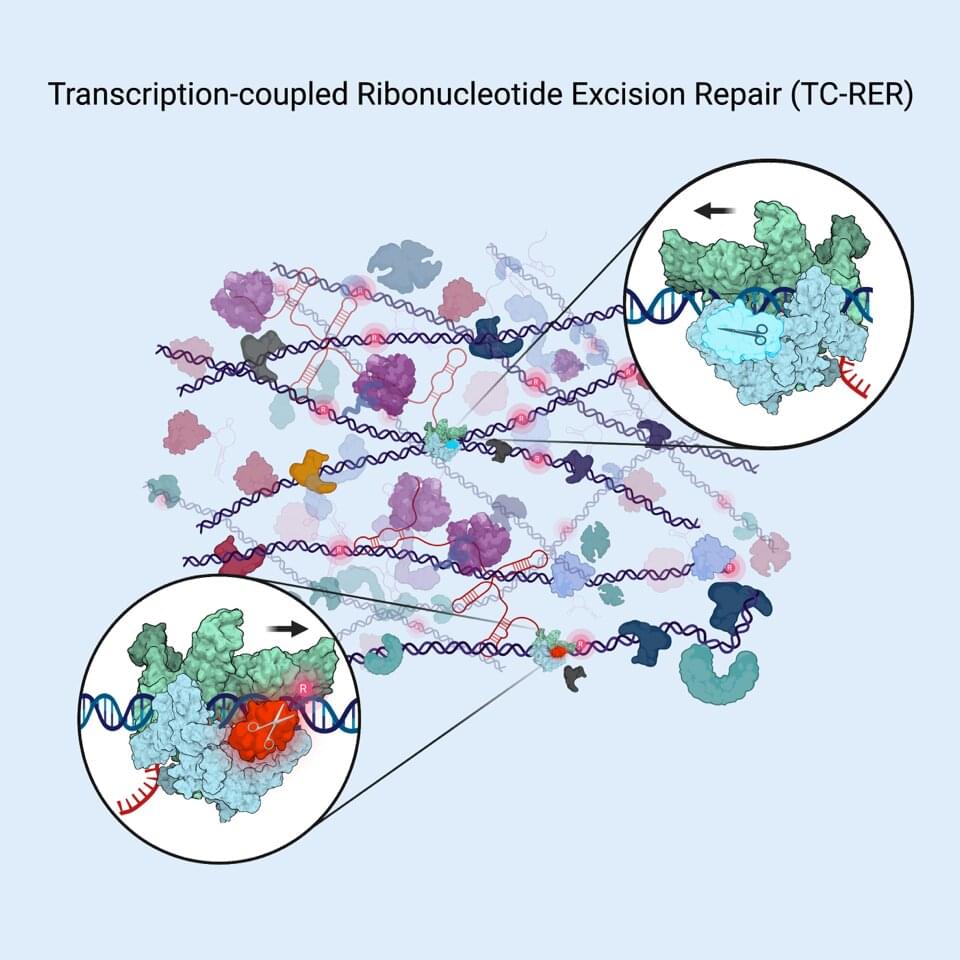
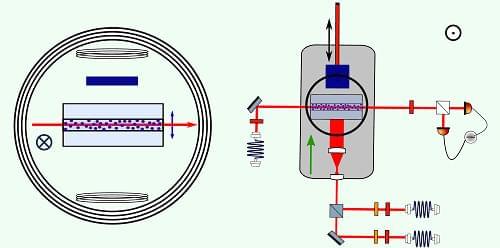
A new study adds to an emerging, radically new picture of how bacterial cells continually repair faulty sections of their DNA.
Published online May 16 in the journal Cell, the report describes the molecular mechanism behind a DNA repair pathway that counters the mistaken inclusion of a certain type of molecular building block, ribonucleotides, into genetic codes. Such mistakes are frequent in code-copying process in bacteria and other organisms. Given that ribonucleotide misincorporation can result in detrimental DNA code changes (mutations) and DNA breaks, all organisms have evolved to have a DNA repair pathway called ribonucleotide excision repair (RER) that quickly fixes such errors.
Last year a team led by Evgeny Nudler, Ph.D., the Julie Wilson Anderson Professor in the Department of Biochemistry and Molecular Pharmacology at NYU Langone Health, published two analyses of DNA repair in living E. coli cells. They found that most of the repair of certain types of DNA damage (bulky lesions), such as those caused by UV irradiation, can occur because damaged code sections have first been identified by a protein machine called RNA polymerase. RNA polymerase motors down the DNA chain, reading the code of DNA “letters” as it transcribes instructions into RNA molecules, which then direct protein building.
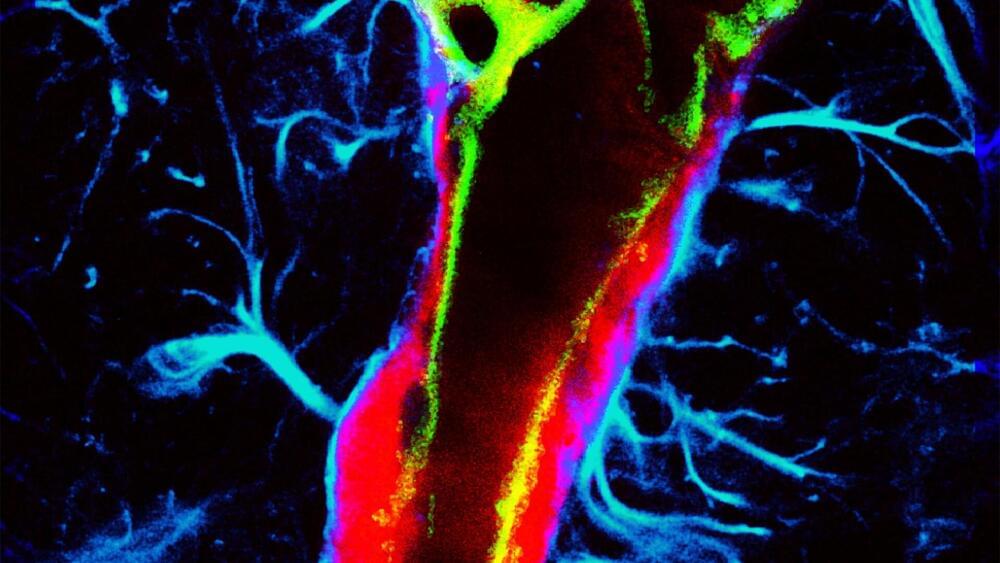
Like the lymphatic system in the body, the glymphatic system in the brain clears metabolic waste and distributes nutrients and other important compounds. Impairments in this system may contribute to brain diseases, such as neurodegenerative diseases and stroke.
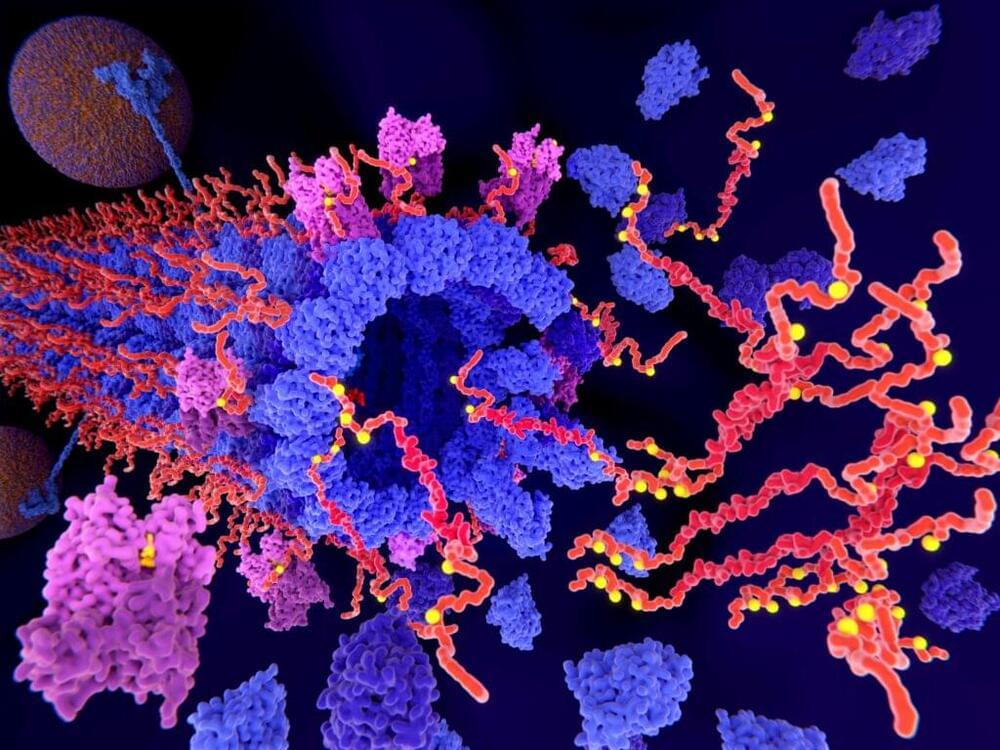
A team of researchers in the McKelvey School of Engineering at Washington University in St. Louis has found a non-invasive and non-pharmaceutical method to influence glymphatic transport using focused ultrasound, opening the opportunity to use the method to further study brain diseases and brain function. Results of the work are published in the Proceedings of the National Academy of Sciences on May 15.
Hong Chen, associate professor of biomedical engineering in McKelvey Engineering and of neurological surgery in the School of Medicine, and her team, including Dezhuang (Summer) Ye, a postdoctoral research associate, and Si (Stacie) Chen, a former postdoctoral research associate, found the first direct evidence that focused ultrasound, combined with circulating microbubbles—a technique they call FUSMB—could mechanically enhance glymphatic transport in the mouse brain.
Scammers are now cloning people’s voices and using it to scam people.
So just hearing them over the phone may not be enough to their identity.
Former FBI special agent Tracy Walder joined “NewsNation Prime” to discuss how to protect yourself from AI phone scams after an Arizona mother received a fake ransom call that used a simulation of her daughter’s voice.
“NewsNation Prime” is America’s source for unbiased news offering a full range of perspectives from across the U.S. Weekends starting at 7p/6C. #Prime.
NewsNation is your source for fact-based, unbiased news for all America.