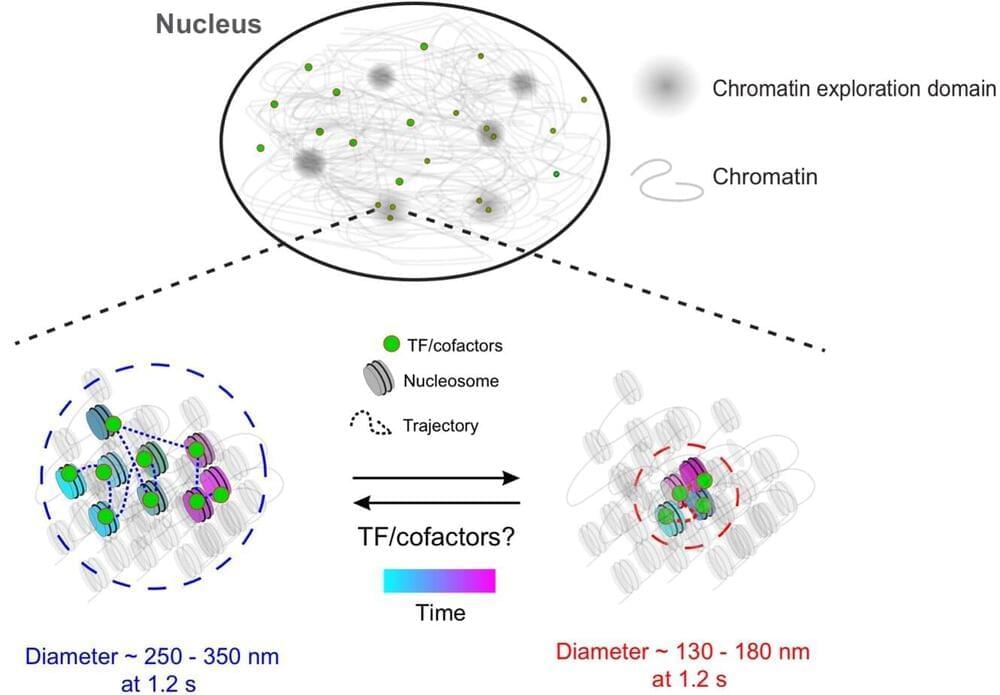
Researchers from Monash University in Melbourne and The University of Western Australia have demonstrated how a reprogramming method imitates embryonic epigenetic reset. Transient naive treatment (TNT) reprogrammed human induced pluripotent stem (hiPS) cells that are molecularly and functionally more similar to human embryonic stem (hES) cells than primed hiPS cells, which are more like cells in the post-implantation embryo. This research suggests that TNT reprogramming has the potential to set a new standard for therapeutic and biomedical uses.
The research article “Transient naive reprogramming corrects hiPS cells functionally and epigenetically” was published online today in Nature.
“Our work shows that TNT reprogramming is a practical and scalable approach to overcome these intrinsic characteristics of hiPS cells, which is important for the clinical delivery of this technology,” stated the authors. “We foresee TNT reprogramming becoming a new standard for biomedical and therapeutic applications.”