Anti-inflammatory drug JAK inhibitors (JAKi) reduces pain in rheumatoid arthritis (RA) but the mechanism is not clear.
To figure out if JAKi directly acted on human sensory neurons, the authors found they expressed JAK1 and STAT3.
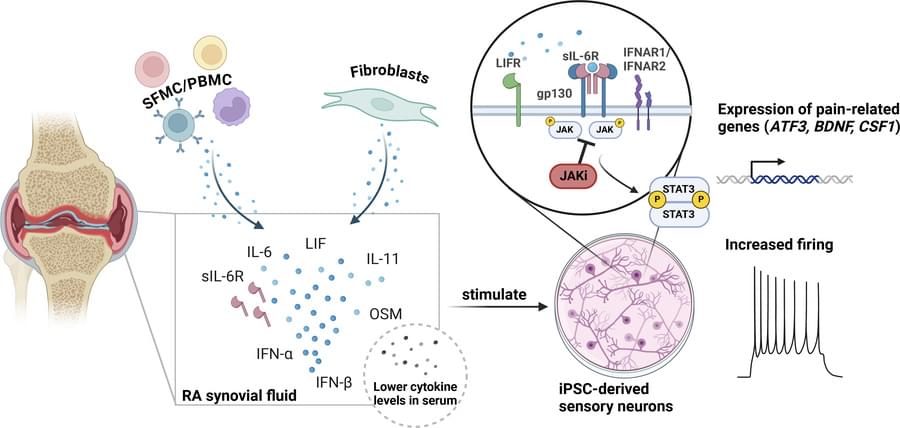
The show that RA synovial fluid addition to human induced pluripotent stem cell (iPSC)-derived sensory neurons led to phosphorylation of STAT3 (pSTAT3), which was completely blocked by the JAKi tofacitinib.
The researchers also discovered that RA synovial fluid was enriched for the STAT3 signalling cytokines IL-6, IL-11, LIF, IFN-alpha and IFN-beta, and their requisite receptors present in peripheral nerves post-mortem.
They observed upregulation of pain-relevant genes with STAT3-binding sites, an effect which was blocked by tofacitinib in cytokine treated iPSCs. LIF also induced neuronal sensitisation, highlighting this molecule as a putative pain mediator.
Tofacitinib reduced the firing rate of sensory neurons stimulated with RA synovial fluid indicating role for JAKi in controlling analgesic properties. https://sciencemission.com/RA-synovial-fluid-induces-JAK-dep…tivation-o
JAK inhibitors (JAKi) are widely used anti-inflammatory drugs. Recent data suggest JAKi have superior effects on pain reduction in rheumatoid arthritis (RA). However, the underlying mechanisms for this observation are not fully understood. We investigated whether JAKi can act directly on human sensory neurons. We analysed RNA sequencing datasets of sensory neurons and found they expressed JAK1 and STAT3. Addition of cell-free RA synovial fluid to human induced pluripotent stem cell (iPSC)-derived sensory neurons led to phosphorylation of STAT3 (pSTAT3), which was completely blocked by the JAKi tofacitinib. Compared to paired serum, RA synovial fluid was enriched for the STAT3 signalling cytokines IL-6, IL-11, LIF, IFN-alpha and IFN-beta, with their requisite receptors present in peripheral nerves post-mortem.