“These neurons are playing an outsized role in hyperglycemia and type 2 diabetes,” said UW Medicine endocrinologist Dr. Michael Schwartz, corresponding author of the paper.
To determine if these neurons contribute to elevated blood sugar in diabetic mice, researchers employed a widely used viral genetics approach to make AgRP neurons express tetanus toxin, which prevents the neurons from communicating with other neurons.
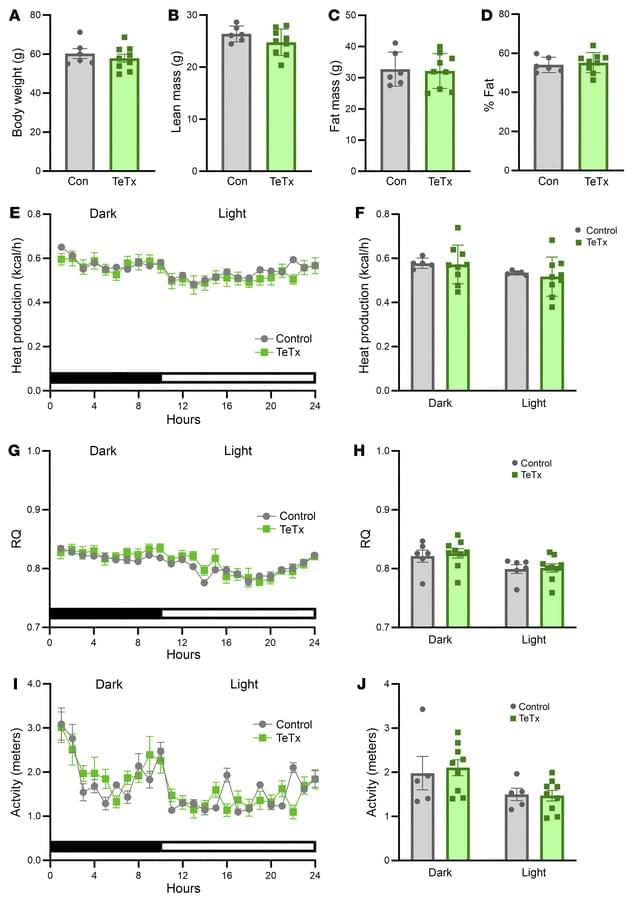
Unexpectedly, this intervention normalized high blood sugar for months, despite having no effect on body weight or food consumption.
Conventional wisdom is that diabetes, particularly type 2 diabetes, stems from a combination of genetic predisposition and lifestyle factors, including obesity, lack of physical activity and poor diet. This mix of factors leads to insulin resistance or insufficient insulin production.
Until now, scientists have traditionally thought the brain doesn’t play a role in type 2 diabetes, according to Schwartz.
The paper challenges this and is a “departure from the conventional wisdom of what causes diabetes,” he said.
The new findings align with studies published by the same scientists showing that injection of a peptide called FGF1 directly into the brain also causes diabetes remission in mice. This effect was subsequently shown to involve sustained inhibition of AgRP neurons.
Together, the data suggest that, while these neurons are important for controlling blood sugar in diabetes, they don’t play a major role in causing obesity in these mice, the researchers noted in their report.
In other words, targeting these neurons may not reverse obesity, even as it causes diabetes to go into remission, Schwartz explained.
More research is needed on how to regulate activity in these neurons, and how they become hyperactive in the first place, he said. Once these questions are answered, Schwartz said that a therapeutic approach might then be developed to calm them down.
This approach could represent a shift in how clinicians understand and treat this chronic disease, Schwartz said. He noted, for instance, that Ozempic and other new drugs used to treat type 2 diabetes are also able to inhibit AgRP neurons.
The extent to which this effect contributes to the antidiabetic action of these drugs is unknown. Further research might help scientists to better understand the role of AgRP neurons in how the body normally controls blood sugar, and to ultimately translate these findings into human clinical trials, he added.
Schwartz holds the UW Robert H. Williams Endowed Chair in Medicine and is a UW professor of medicine, Division of Metabolism, Endocrinology and Nutrition, and an adjunct professor of laboratory medicine and pathology. He is also the founding director of the UW Medicine Diabetes and Obesity Center of Excellence.
AgRP neuron hyperactivity drives hyperglycemia in a mouse model of type 2 diabetes.
1Department of Medicine, University of Washington Medicine Diabetes Institute, Seattle, Washington, USA.
2Ivy Brain Tumor Center, Department of Neurosurgery, Barrow Neurological Institute, Phoenix, Arizona, USA.
3Department of Pediatric Gastroenterology and Hepatology, Seattle Children’s Hospital, Seattle, Washington, USA.