The disability burden for people with multiple sclerosis (MS) can vary significantly depending on whether they have a relapsing/remitting form of the disease, where they experience periods of clinical remission, or a progressive form, where they have continued neurological deterioration without clinical remission. Effective therapies exist for managing relapsing/remitting MS, but treatment for progressive MS has proved more challenging. Now, a new paper published in the journal Brain from researchers at the Advanced Science Research Center (ASRC) at The Graduate Center, CUNY and Friedman Brain Institute at the Icahn School of Medicine at Mount Sinai has identified potential mechanisms that may inform the development of therapies that effectively manage progressive MS.
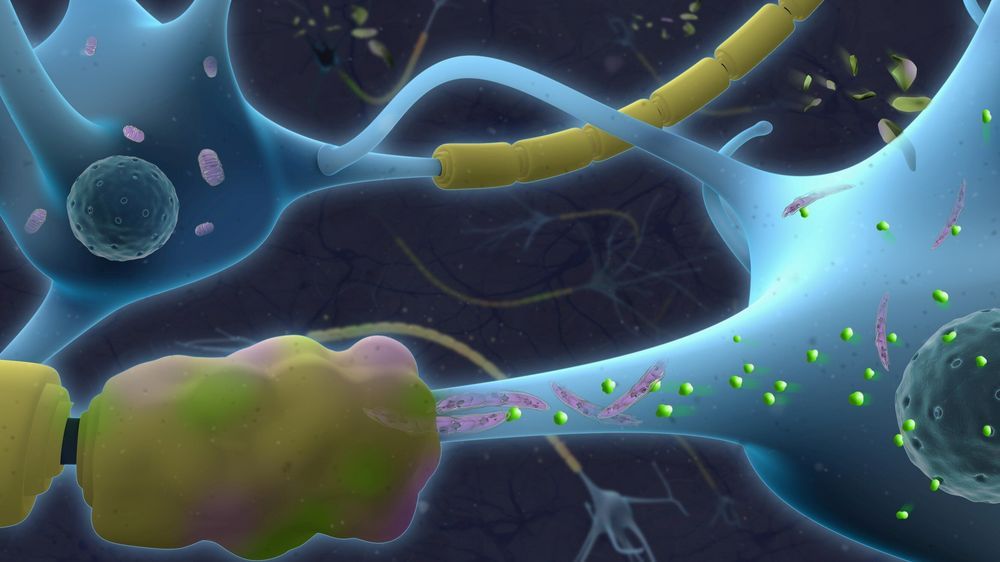
Previous research had suggested that dysfunction of neuronal mitochondria—the energy-producing subcellular organelles—occurs in the brains of MS patients with progressive clinical disability. However, the molecular mechanisms underlying this process remained elusive.
“Because the brain is bathed by the cerebrospinal fluid (CSF), we asked whether treating cultured neurons with the CSF from MS patients with a relapsing/remitting or a progressive disease course would possibly elicit different effects on neuronal mitochondrial function,” said the study’s primary investigator Patrizia Casaccia, Einstein Professor of Biology at The Graduate Center and founding director of the Neuroscience Initiative at the ASRC. “We detected dramatic differences in the shape of the neuronal mitochondria and their ability to produce energy. Only exposure to the CSF from progressive MS patients caused neuronal mitochondria to fuse and elongate while rendering them unable to produce energy. We therefore searched for potential mechanisms of CSF-induced neurodegeneration with the intent to define therapeutic strategies.”