Beneath the moon’s cratered surface lie networks of lava tubes and deep pits, natural caves that could shelter future lunar bases from cosmic radiation and wild temperature swings. These underground structures represent some of the most scientifically valuable areas in the solar system, but they come with the very real challenge of simply getting there.
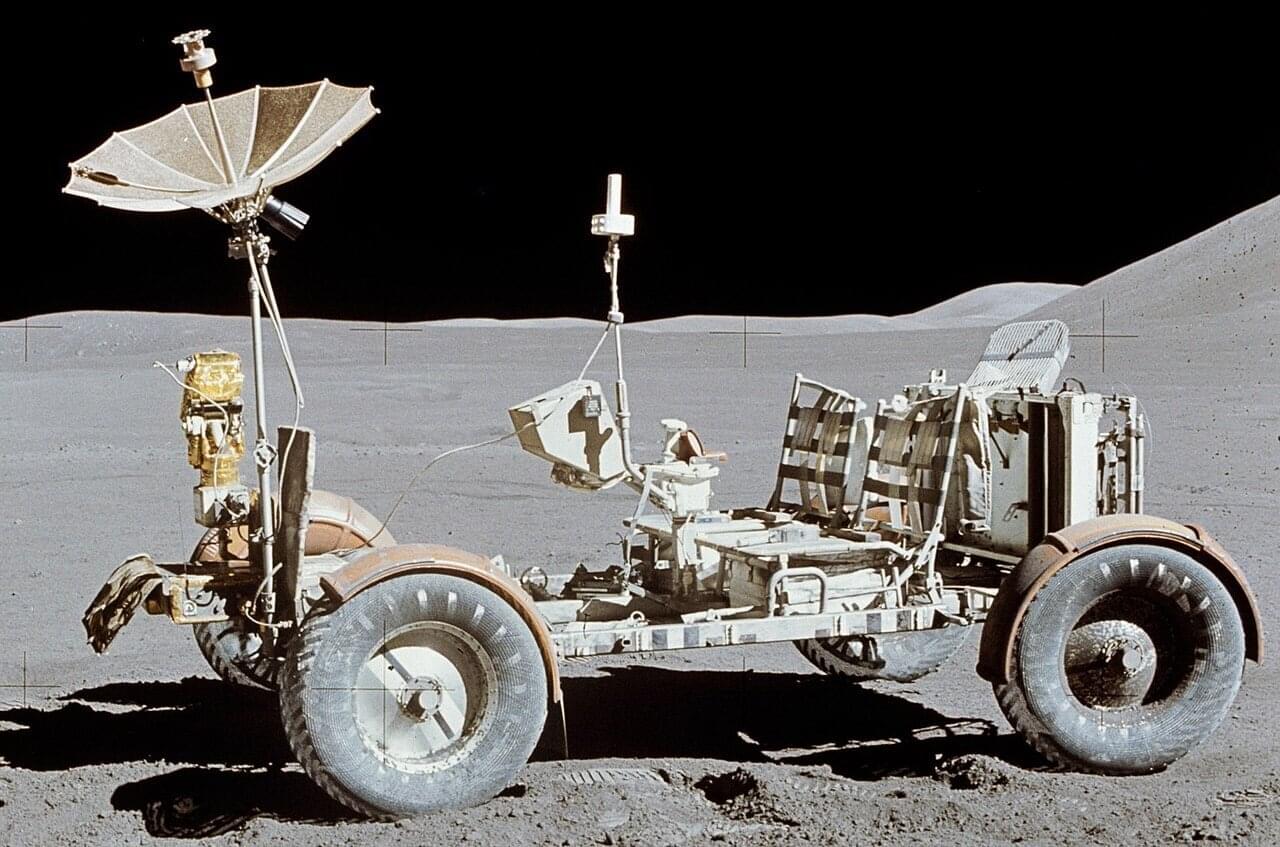
The entrances to these caves feature steep, rugged terrain with rocks and loose regolith. Small rovers, preferred for lunar exploration because you can deploy many of them to reduce mission risk, face an inherent limitation. Their compact wheels simply can’t climb over obstacles much larger than the wheel diameter itself. Send a swarm of small rovers and even if some fail, others continue the mission. Send one large rover and a single failure ends everything.
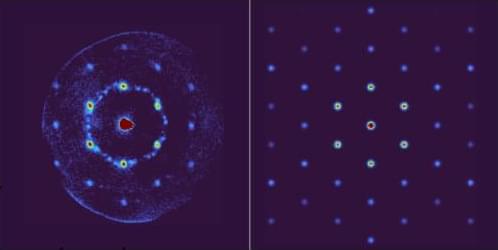
Variable diameter wheels are a new thing in lunar exploration and could solve this, expanding when needed to overcome obstacles, then contracting for efficient transport. But building such a wheel for the moon has proven nearly impossible. The lunar environment is uniquely hostile to mechanical systems. Fine, abrasive dust infiltrates everything, and in the airless vacuum, exposed metal surfaces stick together through a process called cold welding. Traditional hinges and joints don’t last long under these conditions.