Physicists have made a substantial breakthrough in understanding subatomic physics by measuring a second mechanical property of protons: the shear force experienced internally. Protons and the… Continue Reading →
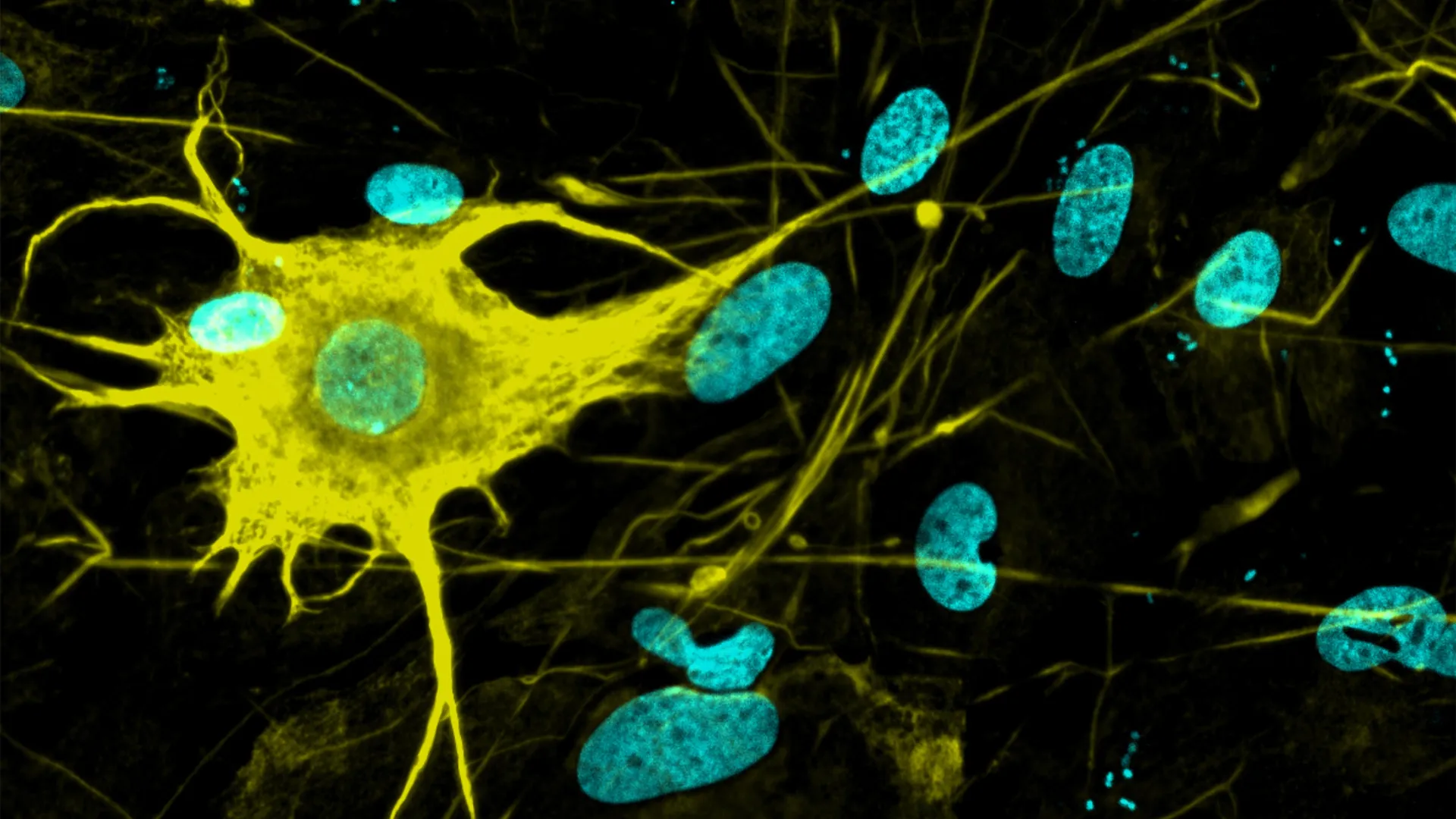
Scientists at ETH Zurich have broken new ground by generating over 400 types of nerve cells from stem cells in the lab, far surpassing previous efforts that produced only a few dozen. By systematically experimenting with combinations of morphogens and gene regulators, the researchers replicated the vast diversity of neurons found in the human brain. This breakthrough holds major promise for studying neurological diseases like Alzheimer’s and Parkinson’s, creating more accurate models for drug testing, and eventually even enabling neuron replacement therapies.
IN A NUTSHELL 🌌 The Quipu superstructure, spanning over 1.3 billion light-years, is the largest known entity in the universe. 🔭 Astronomers utilize X-ray galaxy clusters to map and analyze these massive cosmic formations. 📊 The immense size of superstructures like Quipu can distort critical cosmological measurements, affecting our understanding of the universe’s expansion. ⏳
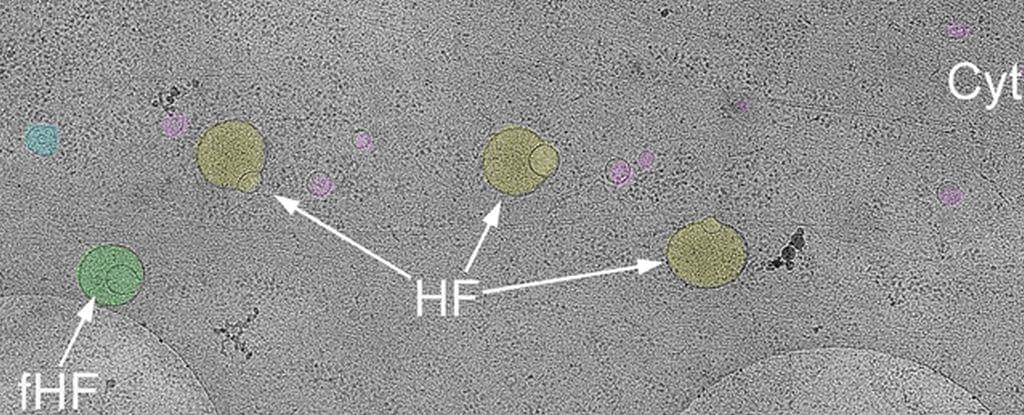
After centuries of mapping the human body in ever-finer detail, scientists are still making discoveries. Here we are, in 2025, and a previously unknown cellular structure that could be vital to our health has just been added to the anatomy books.
The membrane-bound organelle appears to play a huge role in helping cells sort, discard, and recycle their contents. It’s called a hemifusome, and a team of scientists says it could shed new light on disease.
“This is like discovering a new recycling center inside the cell,” said biophysicist Seham Ebrahim of the University of Virginia. “We think the hemifusome helps manage how cells package and process material, and when this goes wrong, it may contribute to diseases that affect many systems in the body.”


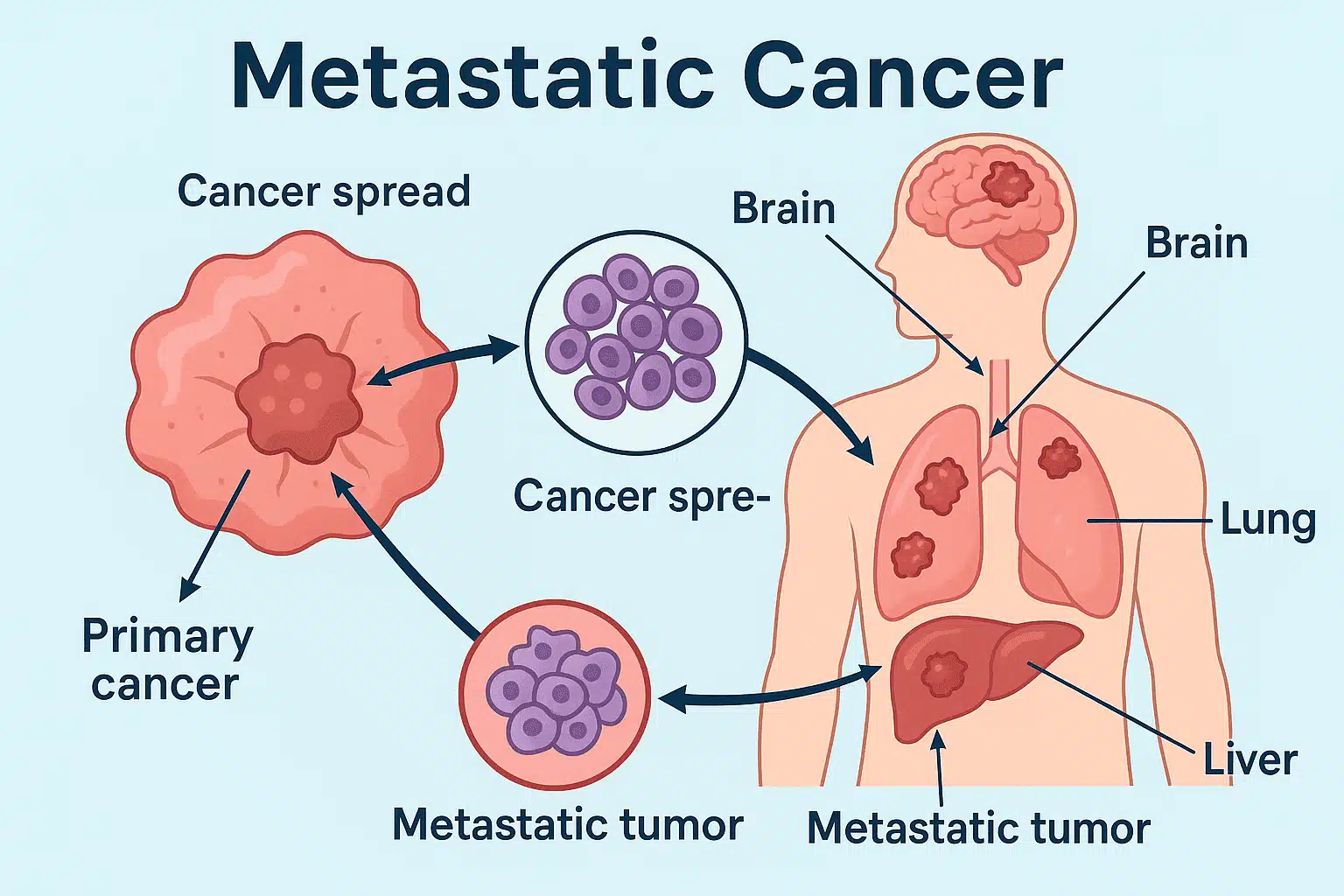
In all patients, the median overall survival (OS) was 10.2 months (95% CI, 8.5−12.2); there was a total of 20 neurologic deaths compared with 64 non-neurologic deaths. Between the 2 reviewers, agreement was 98% regarding neurologic death and non-neurologic death, with disagreement requiring a tie occurring in 2%.
The 1-year and 2-year neurologic death incidence was 11.0% (95% CI, 5.8%-18.1%) and 20.3% (95% CI, 12.7%-29.1%), respectively. The trial investigators noted that the historical incidence of neurologic death with WBRT was 17.5% at 1 year and 35.2% at 2 years. The 1-year and 2-year incidence of non-neurologic death was 48.0% (95% CI, 37.9%-57.4%) and 61.7% (95% CI, 50.8%-70.8%).
Via the Fine and Gray regression analysis, age, number of brain metastases, size of largest brain metastases, presence of neurologic symptoms, presence of distant extracranial metastases, and employment of neurological resection before enrollment were not associated with neurological death (P .05 in all cases).
New brain metastases were developed by 61.0% of patients, with a 1-year estimate of 59.0% (95% CI, 48.6%-68.0%); at least 1 course of salvage stereotactic radiation was received by 39.0% of patients, with a 1-year estimate of 37.0% (95% CI, 27.5%-46.5%); WBRT was received by 22.0%, with a 1-year estimate of 21.0% (95% CI, 13.6%-29.5%); and leptomeningeal disease was observed in 9.0%, with a 1-year estimate of 7.0% (95% CI, 3.1%-13.1%).
Overall, systemic disease progression occurred in 65.0% of patients, with a 1-year estimate of 58% (95% CI, 47.6%-67.0%).
Additionally, in aggregate, at least 1 local recurrence in a metastasis treated in the study was experienced by 13.0%, with a 1-year estimate of 15.0% (95% CI, 8.8%-22.7%); the respective per-patient rates of radiographic and symptomatic necrosis were 9.0% and 5.0% in total, with 1-year estimates of 6.0% (95% CI, 2.4%-11.9%) and 3.0% (95% CI, 0.8%-7.9%), respectively.
“Despite being the historical standard, whole brain radiation might not be necessary for all patients,” stated first study author Ayal Aizer, MD, MHS, director of Central Nervous System Radiation Oncology at Brigham and Women’s Hospital, and a founding member of the Mass General Brigham healthcare system, in a press release on the study.2 “Our findings demonstrate that targeted, brain-directed radiation may be a viable treatment for patients with limited brain metastases from SCLC and potentially spare them from the [adverse] effects of whole brain radiation.”