
Get the latest international news and world events from around the world.

Scientists Chasing Artificial Kidneys Create Most Complex Kidney Tissue Yet
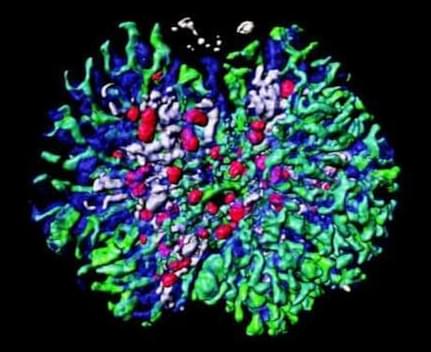
The team noted that although other studies have been able to create nephrons and ureteric ducts from stem cells, these didn’t fully function as they would in real kidneys due to the absence of stromal cells, which are crucial for cell signaling. The team took embryonic stem cells from mice and induced these to differentiate into kidney-specific stromal cells, using a cocktail of chemicals meant to mimic those that would occur in vivo.
When they combined the stromal cells with nephron and ureteric bud cells (which they also created from stem cells), the result was a “kidney-like 3D tissue, consisting of extensively branched tubules and several other kidney-specific structures.”
According to the researchers, this is the most complex kidney structure that’s been generated from scratch in a lab. Though this study was done in mice, the team noted that it has already created the first two kidney components—nephron progenitors and ureteric buds—from human induced pluripotent stem cells (iPSCs). If they’re able to also create stromal cells from iPSCs, they said, “a similarly complex human kidney should be achievable.”
A new type of killer T-cell can stop attacks on healthy tissue
A team of scientists has discovered a brand new form of human T cell that suppresses attacks on healthy tissues, which could lead to treatments for illnesses ranging from lupus to cancer.
In case you forgot, T cells are one of the most significant white blood cells in the immune system, playing a crucial role in adaptive immune response. They can kill diseased or malignant cells; however, studies in mice have shown that some of these cells may also kill T cells responsible for orchestrating autoimmune responses.
For years, scientists have believed that humans share the same cells, but until now, no one had been able to verify their existence.

Scientists “Elated”
An international team of researchers claim to have slowed the signs of aging in mice by resetting their cells to younger states, using a genetic treatment.
To the scientists, The Guardian reports, it’s a breakthrough in cell regeneration and therapeutic medicine that doesn’t seem to cause any unexpected issues in mice.
“We are elated that we can use this approach across the life span to slow down aging in normal animals,” said Juan Carlos Izpisua Belmonte, Salk Institute professor and co-corresponding author of a new study published in the journal Nature Aging, in a statement. “The technique is both safe and effective in mice.”

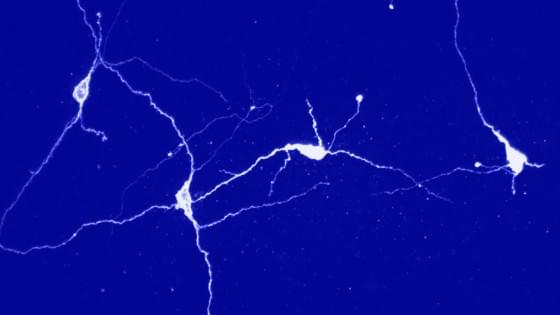
Optogenetics reveals new insights into circuits of the brain
To date, scientists have largely been in the dark with regard to how individual circuits operate in the highly branched networks of the brain. Mapping these networks is a complicated process, requiring precise measurement methods. For the first time, scientists from the Max Planck Institute for Biological Cybernetics in Tübingen, Germany, together with researchers from the Ernst Strüngmann Institute in Frankfurt and Newcastle University in England, have now functionally proven a so far poorly understood neural connection in the visual system of monkeys using optogenetic methods. To this end, individual neurons were genetically modified so that they became sensitive to a light stimulus.
For decades microstimulation was the method of choice for activating neurons – the method proved to be reliable and accurate. That is why it is also used medically for deep brain stimulation. The Tübingen-based scientists were now able to show that optogenetics, a biological technique still in its infancy, delivers comparable results.
With optogenetics it is possible to directly influence the activity of neurons by light. To do this individual neurons are genetically modified with the help of viruses to express light-sensitive ion channels in their cell membrane. Through blue light pulses delivered directly into the brain, the modified neurons can then be systematically activated.
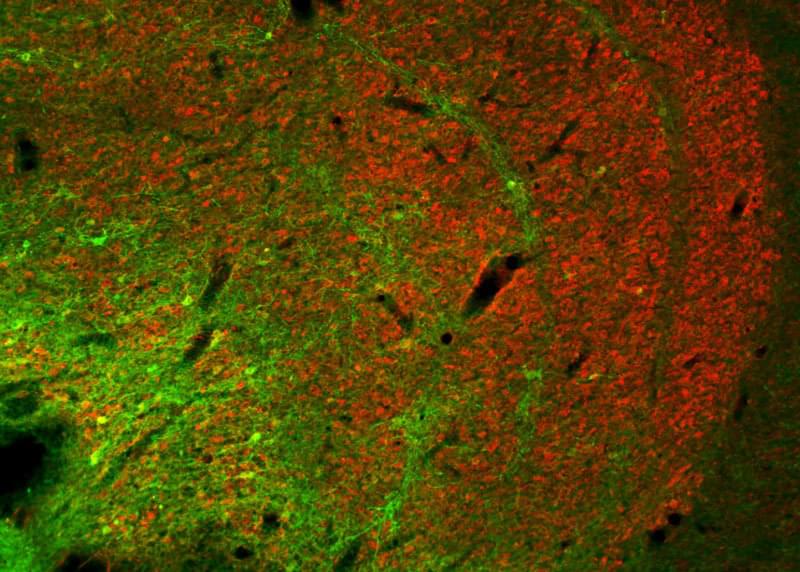
Scientists cast light on the brain’s social cells
Picture yourself hovering over an alien city with billions of blinking lights of thousands of types, with the task of figuring out which ones are connected, which way the electricity flows and how that translates into nightlife. Welcome to the deep brain.
Even in an era rapidly becoming known as the heyday of neuroscience, tracing the biochemical signaling among billions of neurons deep in the brain has remained elusive and baffling.
A team of Stanford University researchers managed to map out one such connection, buried inside the brain of a living, moving mammal as they manipulated its behavior. The feat offers an unprecedented close-up of the genesis of social behavior on a cellular level, and could offer insights into psychiatric puzzles such as autism, depression and anxiety.

Study charts development of emotional control in teens
In the midst of all the apparent tumult, intense emotion, and occasional reckless behavior characterizing the teenage years, the brain is, in fact, evolving and developing the neural circuits needed to keep emotions in check. Research in the June 8, 2016 issue of The Journal of Neuroscience describes how the ability to control emotions moves from one brain area to another as teens mature into adults, offering an opportunity to understand how disorders related to emotional control emerge.
“Our study opens the way for a better understanding of the neurobiology behind adolescent behavior in emotionally arousing situations,” said study author Anna Tyborowska of Radboud University Nijmegen in the Netherlands. “The findings could also have important clinical implications [as] many psychiatric disorders emerge during adolescence and are characterized by problems with emotional action control.”
Previous research links the spike in sensation-seeking and impulsive behavior during adolescence to the delayed maturation of the prefrontal cortex, a region of the brain involved in reasoning, planning, and decision-making. Study authors Inge Volman, Ivan Toni, and Karin Roelofs previously demonstrated the importance of the anterior prefrontal cortex in emotional control in adults. However, it has not been clear whether and how the delayed development of the prefrontal cortex affects emotional control during adolescence.
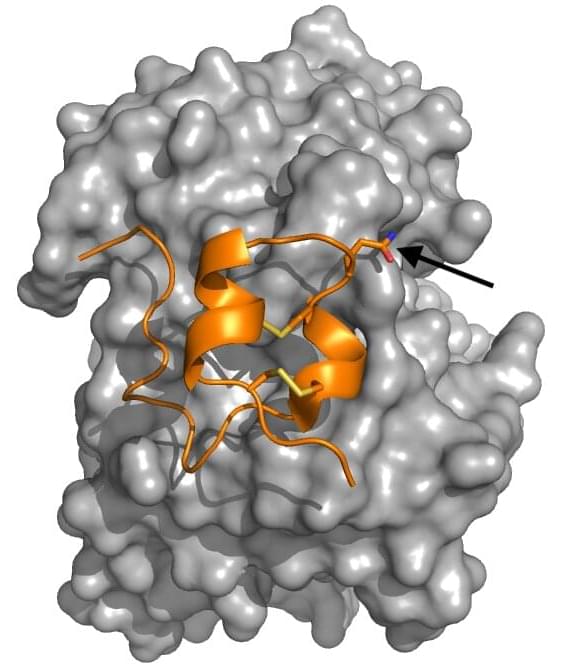
New study confirms bioengineered RSV protein vaccine evokes protective immune response
Close interactions with infectious disease set both University of California, Santa Cruz graduate student Ana Nuñez Castrejon and Associate Professor of Biomolecular Engineering Rebecca DuBois on the path of studying respiratory syncytial virus (RSV), a common and sometimes dangerous respiratory disease for which there is not currently a vaccine. The two researchers recently marked a major milestone in their effort to create an effective vaccine for the virus with the publishing of their paper “Structure-based design and antigenic validation of respiratory syncytial virus G immunogens” in the Journal of Virology.
For fifth-year Baskin Engineering student and the paper’s lead author Nuñez Castrejon, a bout of pneumonia that lingered for months when she was an undergraduate student sparked her interest in studying respiratory illnesses. For DuBois, watching her child go through a serious infection of RSV, which can cause severe respiratory infections in infants/children and the elderly, led her to study the disease.
“We have all of these wonderful childhood vaccines that have eliminated so much childhood disease, but there are still a lot of infectious diseases that are really tough on children, and RSV is one of those that causes hospitalizations in children,” DuBois said.
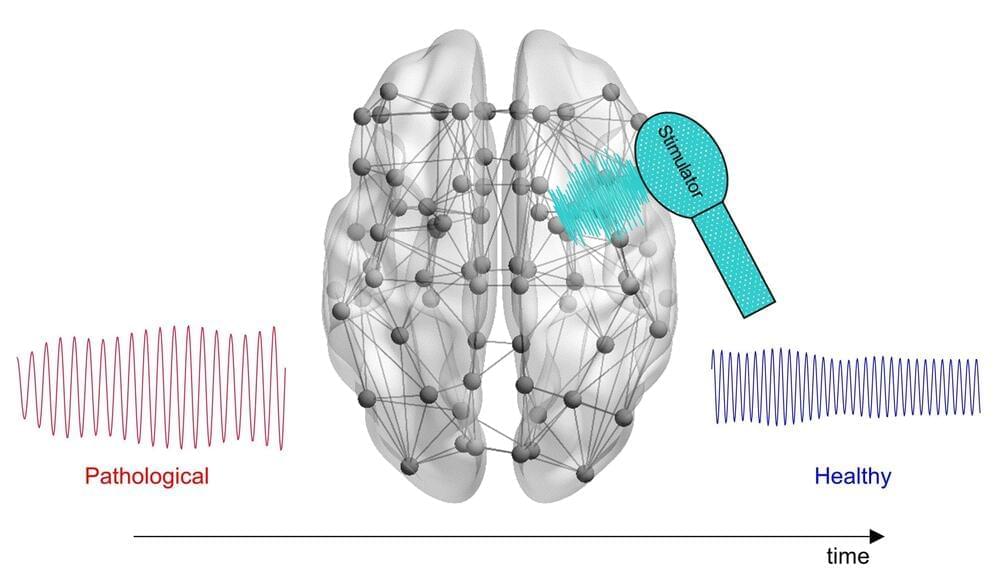
New computational tool could help optimize treatment of Alzheimer’s disease
Scientists have developed a novel computational approach that incorporates individual patients’ brain activity to calculate optimal, personalized brain stimulation treatment for Alzheimer’s disease. Lazaro Sanchez-Rodriguez of the University of Calgary, Canada, and colleagues present their new framework in PLOS Computational Biology.
Electrical stimulation of certain parts of the brain could help promote healthy activity in neural circuits impaired by Alzheimer’s disease, a neurodegenerative condition. This experimental treatment has shown some promise in clinical trials. However, all patients currently receive identical treatment protocols, potentially leading to different outcomes according to individual variations in brain signaling.
To investigate the possibility of personalized brain stimulation, Sanchez-Rodriguez and colleagues took a theoretical approach. They built a computational tool that incorporates patients’ MRI scans and physiological brain signaling measurements to calculate optimal brain stimulation signals, with the goal of delivering efficient, effective personalized treatment.