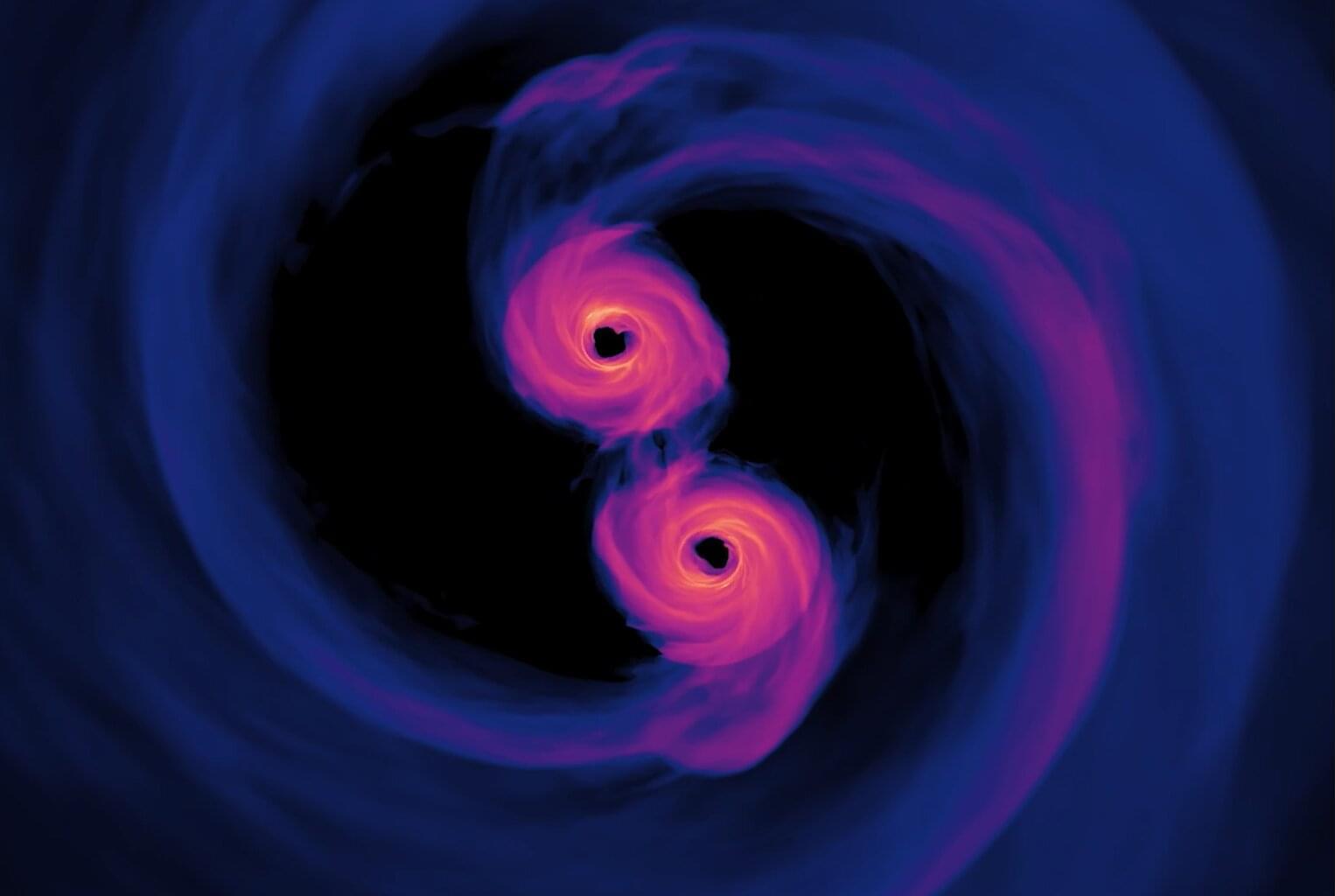
An international collaboration of astrophysicists that includes researchers from Yale has created and tested a detection system that uses gravitational waves to map out the locations of merging black holes—known as supermassive black hole binaries—around the universe. Such a map would provide a vital new way to explore and understand astronomy and physics, just as X-rays and radio waves did in earlier eras, the researchers say. The new protocol demonstrated by the North American Nanohertz Observatory for Gravitational Waves (NANOGrav) offers a detection protocol to populate the map.
“Our finding provides the scientific community with the first concrete benchmarks for developing and testing detection protocols for individual, continuous gravitational wave sources,” said Chiara Mingarelli, assistant professor of physics in Yale’s Faculty of Arts and Sciences (FAS), member of NANOGrav, and corresponding author of a new study published in The Astrophysical Journal Letters.
According to the researchers, even a small number of confirmed black hole binaries will enable them to anchor a map of the gravitational wave background. In the months ahead, NANOGrav will continue identifying and locating binaries.