Artificial intelligence (AI) is a foundational technology that could reshape our world, driving new scientific discoveries and helping us tackle humanity’s greatest challenges. Now, we’re asking where we can go to unlock its fullest potential.
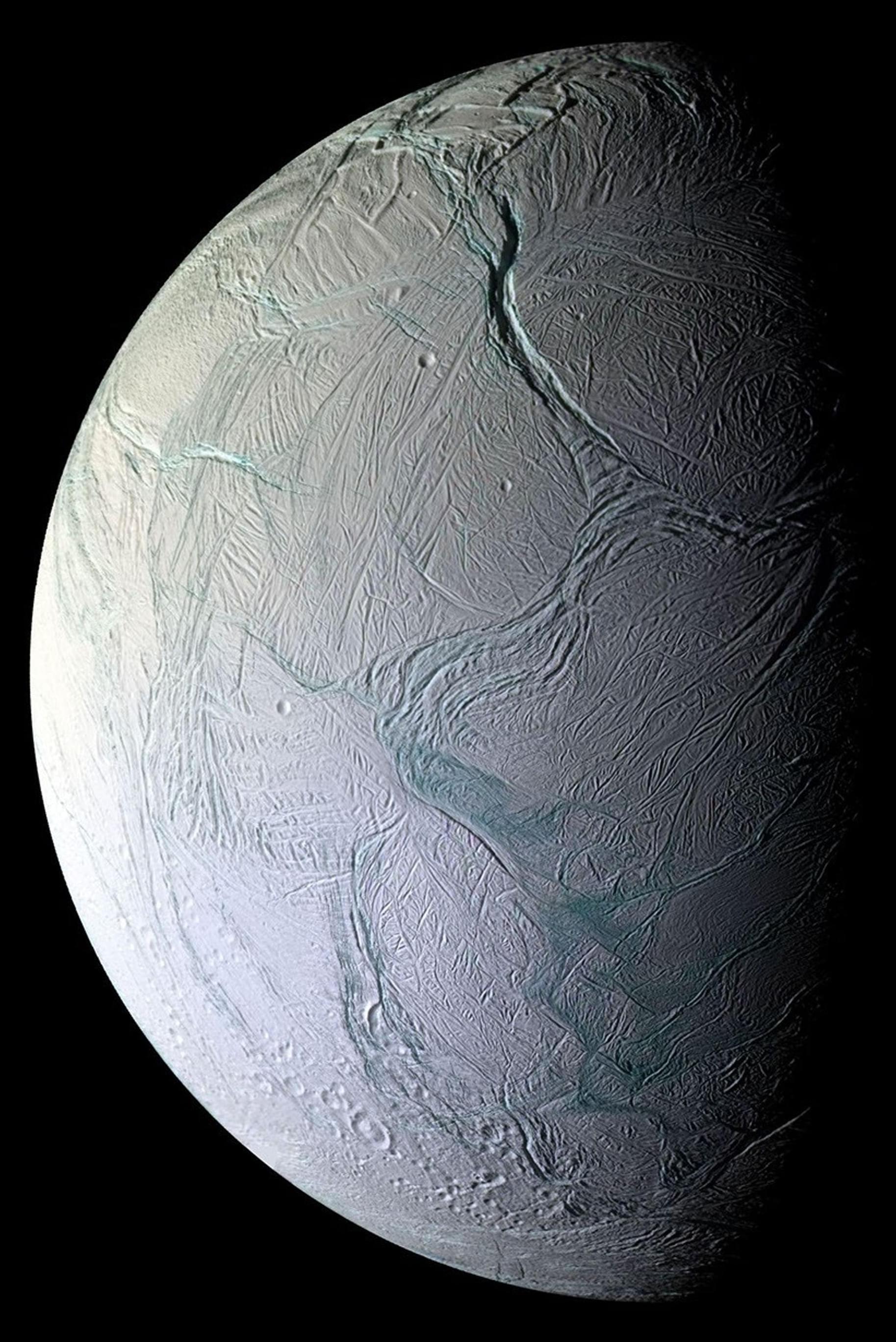
The Sun is the ultimate energy source in our solar system, emitting more power than 100 trillion times humanity’s total electricity production. In the right orbit, a solar panel can be up to 8 times more productive than on earth, and produce power nearly continuously, reducing the need for batteries. In the future, space may be the best place to scale AI compute. Working backwards from there, our new research moonshot, Project Suncatcher, envisions compact constellations of solar-powered satellites, carrying Google TPUs and connected by free-space optical links. This approach would have tremendous potential for scale, and also minimizes impact on terrestrial resources.
We’re excited about this growing area of exploration, and our early research, shared today in “Towards a future space-based, highly scalable AI infrastructure system design,” a preprint paper, which describes our progress toward tackling the foundational challenges of this ambitious endeavor — including high-bandwidth communication between satellites, orbital dynamics, and radiation effects on computing. By focusing on a modular design of smaller, interconnected satellites, we are laying the groundwork for a highly scalable, future space-based AI infrastructure.