‘You’re in a world made of marshmallows!’
A Google app that allows people to communicate with artificial intelligence (AI) systems has been made available in the United Kingdom (U.K.) for a limited trial period.
You’re in a world made of marshmallows! As you take a step, a gentle ‘squish’ comes out under your feet. The marshmallow horizon stretches out in all directions. The sky is a gooey, sticky pink.
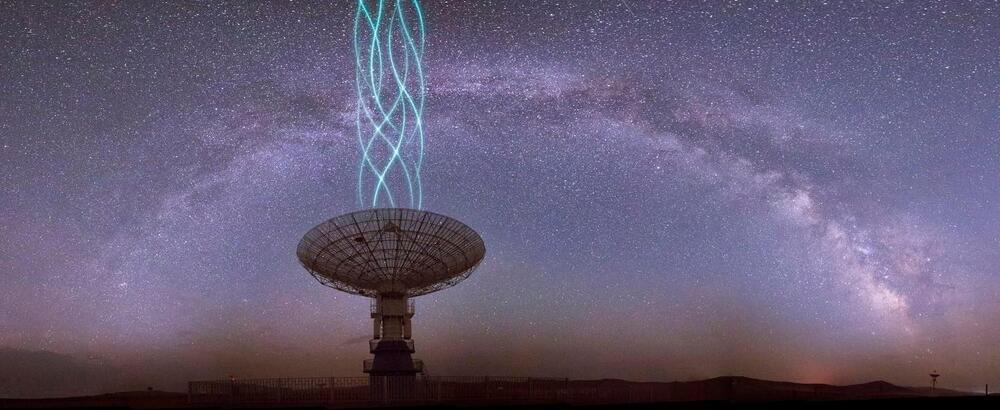
Andrey Suslov/iStock.
The app called AI Test Kitchen App made for experimenting with Google’s Language Model for Dialogue Applications (LaMDA), conversational AI, cannot learn new skills from users, although it welcomes comments on how it functions, BBC reported on Wednesday.