In the last decade, the incidence of restrictive eating disorders in children, like anorexia-nervosa and avoidant/restrictive food intake disorders (ARFID), has doubled. These disorders have severe consequences for growing children, resulting in nutritional deficiencies and problems with bone development, statural growth and puberty. Most studies have focused on the effects of these disorders in older individuals, and little is currently known about how restrictive eating disorders affect the brain in children or what mechanisms in the brain might be responsible for this restrictive eating behavior.
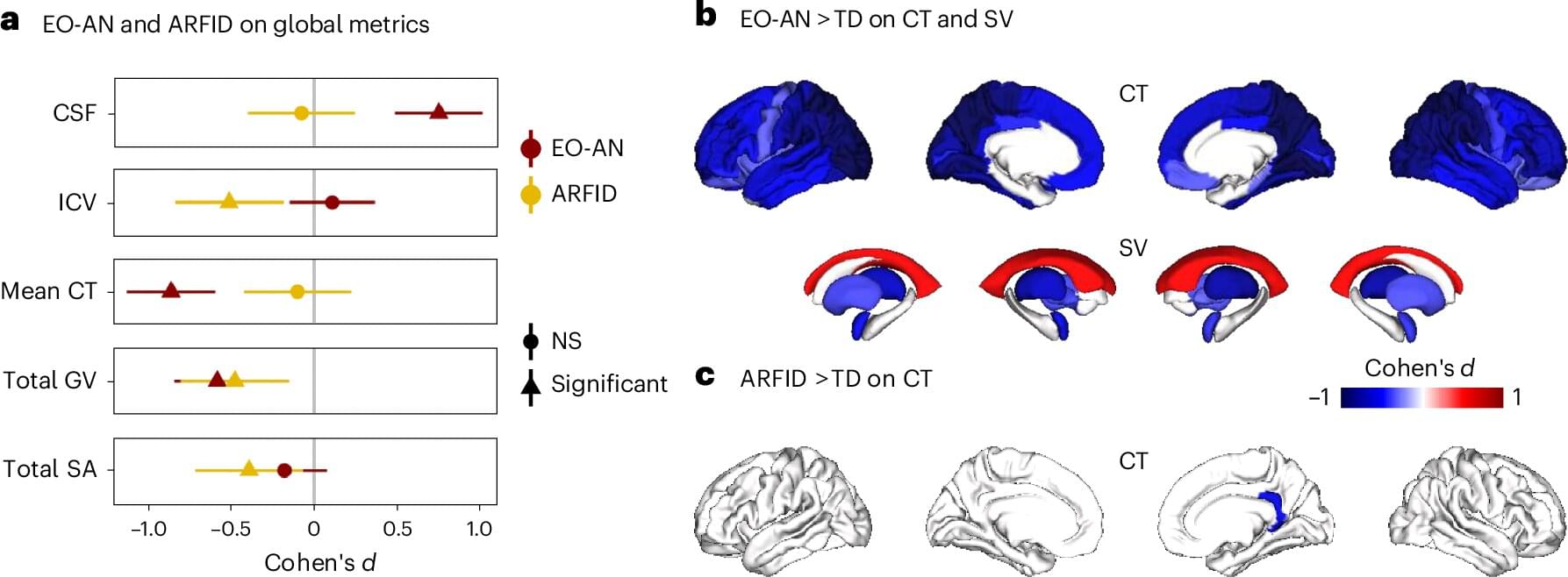
To get a better understanding of how these early-onset eating disorders work in the brain, researcher Clara Moreau and her team conducted MRI brain scans on 290 children, of which 124 had been hospitalized for early-onset anorexia-nervosa (EO-AN), 50 had been hospitalized for ARFID, and 116 were children with no eating disorders. All participants were under 13 years old, and those who were hospitalized had very low body mass index (BMI) due to restrictive eating. The results were published in Nature Mental Health.
Although EO-AN and AFRID both result in low BMI and malnutrition due to restrictive eating, they are distinct disorders. EO-AN—as well as later onset anorexia-nervosa—is characterized by restrictive eating arising from a distorted body image, while restrictive eating in AFRID arises from sensory issues, such as a dislike of certain food textures, a lack of interest in food or fear of negative health consequences from food. These differences indicate that the disorders probably arise from different mechanisms in the brain.