Once we arrive at AGI (artificial general intelligence), the pursuit of ASI (artificial superintelligence) is next. Here is a speculated timeline 2040–2050.


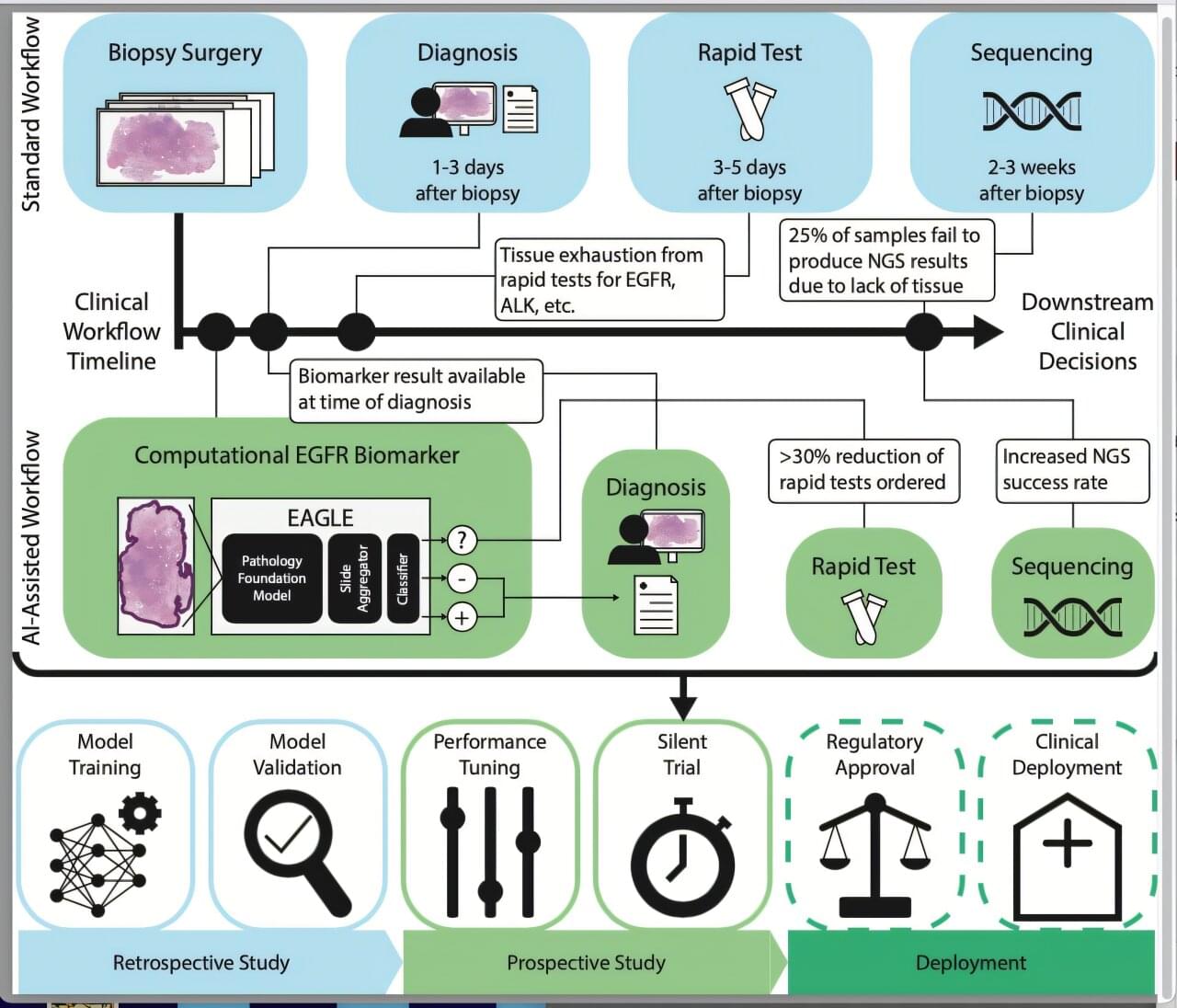
A new study by researchers at the Icahn School of Medicine at Mount Sinai, Memorial Sloan Kettering Cancer Center, and collaborators, suggests that artificial intelligence (AI) could significantly improve how doctors determine the best treatment for cancer patients—by enhancing how tumor samples are analyzed in the lab.
The findings, published in Nature Medicine, showed that AI can accurately predict genetic mutations from routine pathology slides—potentially reducing the need for rapid genetic testing in certain cases.
The paper is titled “Enhancing Clinical Genomics in Lung Adenocarcinoma with Real-World Deployment of a Fine-Tuned Computational Pathology Foundation Model.”
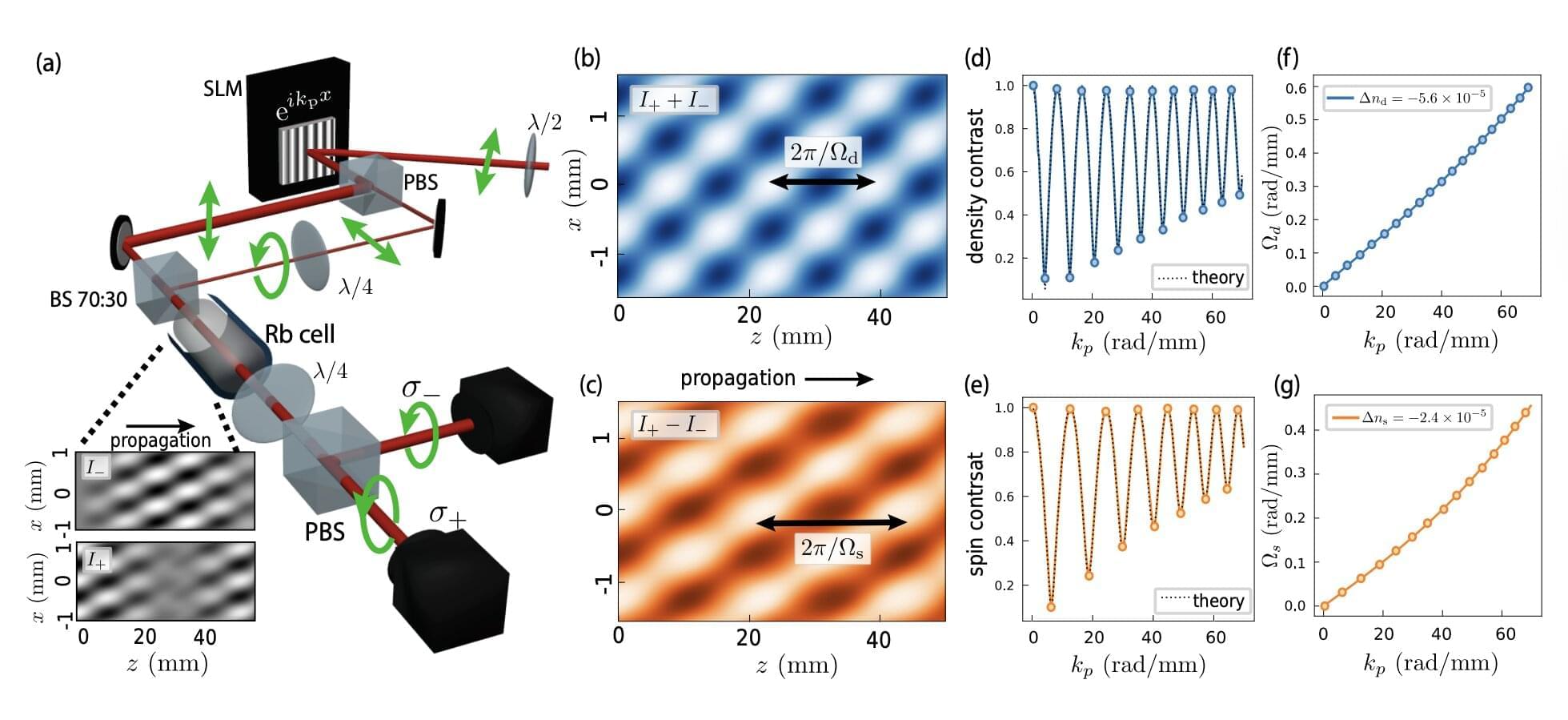
Recent physics studies have found that light can sometimes flow in unexpected ways, behaving like a so-called “superfluid.” Superfluids, such as ultracold atomic gases or helium-4 below specific temperatures, are phases of matter characterized by flowing behavior with zero viscosity (i.e., with no resistance).

Researchers at Princeton University and the Simons Foundation have identified four clinically and biologically distinct subtypes of autism, marking a transformative step in understanding the condition’s genetic underpinnings and potential for personalized care.
Analyzing data from over 5,000 children in SPARK, an autism cohort study, the researchers used a computational model to group individuals based on their combinations of traits.
The team used a “person-centered” approach that considered a broad range of over 230 traits in each individual, from social interactions to repetitive behaviors to developmental milestones, rather than searching for genetic links to single traits.

Even in moderation, consumption of ultra-processed foods is linked with measurable increases in risk for chronic diseases, according to research from the Institute for Health Metrics and Evaluation at the University of Washington. Processed meat, sugar-sweetened beverages (SSBs), and trans fatty acids (TFAs) were associated with an increased disease risk, such as type 2 diabetes, ischemic heart disease (IHD), and colorectal cancer.
Multiple previous studies have linked ultra-processed foods, particularly processed meats, sugar-sweetened beverages, and trans fatty acids, with elevated chronic disease risks. Estimates suggest that diets high in processed meat contributed to nearly 300,000 deaths worldwide in 2021, while diets rich in sugar-sweetened beverages and trans fats accounted for millions of disability-adjusted life years.
Processed meats preserved through smoking, curing or chemical additives often contain compounds such as N-nitroso agents, polycyclic aromatic hydrocarbons and heterocyclic amines—compounds implicated in tumor development.
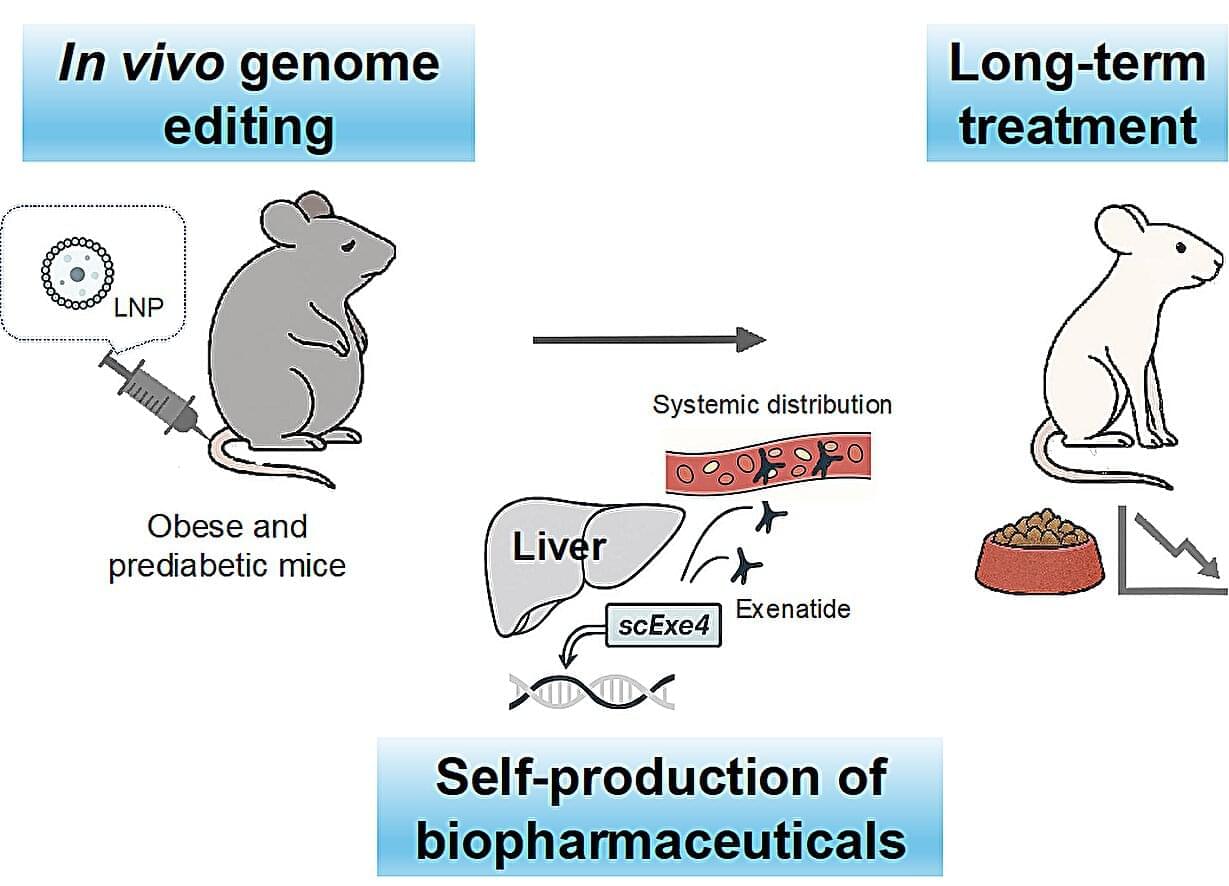
Weight-loss drugs have surged in popularity, promising rapid results with regular injections. Now, researchers from Japan report a way for the body to make its own weight-loss drugs, doing away with injections in favor of a one-time treatment.
In the study, “Targeted In Vivo Gene Integration of a Secretion-Enabled GLP-1 receptor agonist Reverses Diet-induced Non-genetic Obesity and Pre-diabetes,” published in Communications Medicine, researchers from the University of Osaka reveal a modified genome editing approach to tackle noncommunicable, multifaceted diseases.
The approach introduced a new protein-coding gene, rather than attempting to correct a mutation in an existing gene and could be the key to lifelong effective weight management.
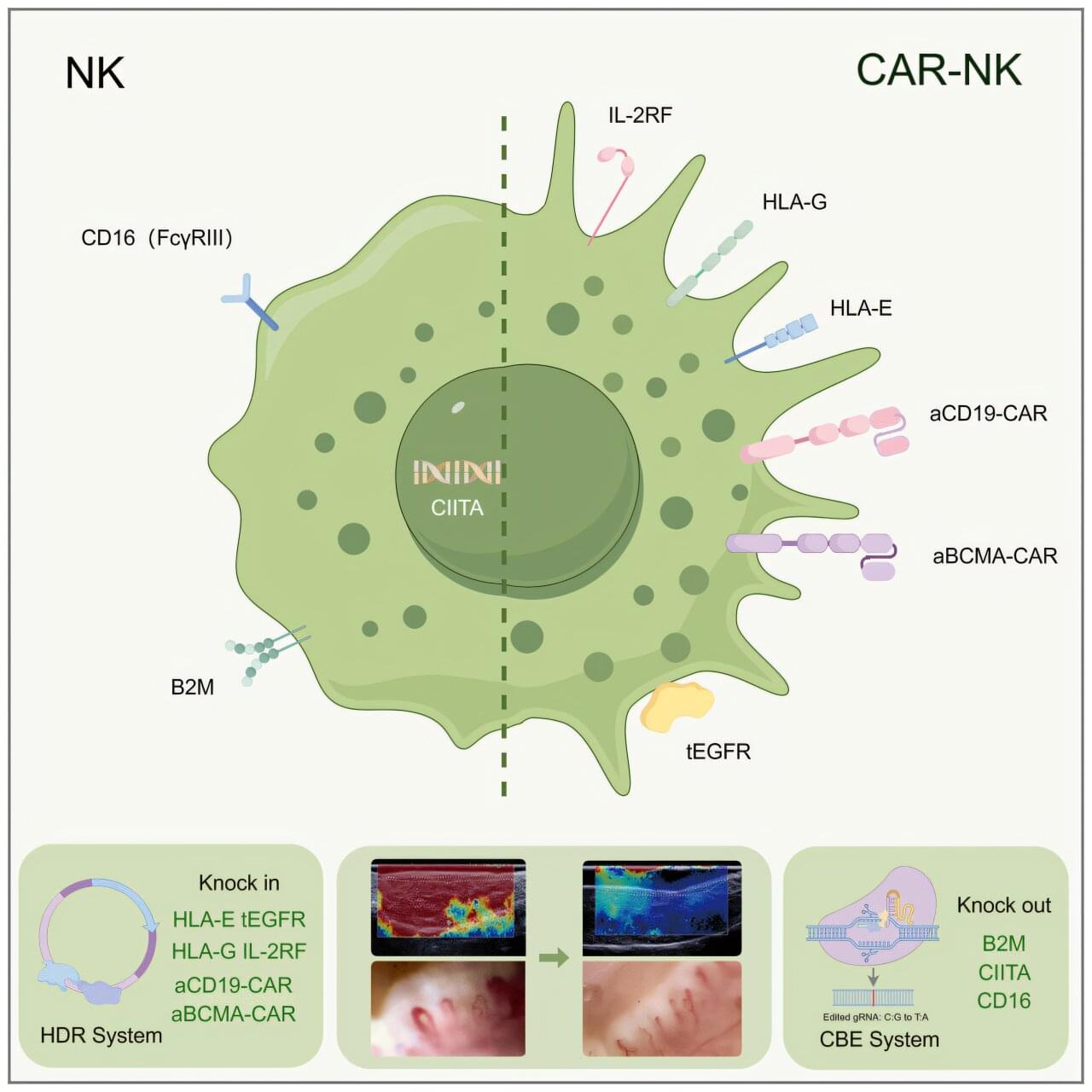
Research led by Naval Medical University’s Changzheng Hospital in China reports that an off-the-shelf cell therapy built from induced pluripotent stem cells (iPSCs) loosened life-limiting skin and organ scarring in a woman with systemic sclerosis.
Systemic sclerosis progressively suffocates tissue through immune misfires, collapsed micro-vessels, and runaway collagen conditions that resist standard immunosuppressants, biologics, and anti-fibrotic drugs while driving a 40% 10-year mortality.
Cell-based approaches such as hematopoietic-stem-cell transplants and CAR-T therapies have shown promise but carry high toxicity or labor-intensive custom manufacturing, leaving clinicians and patients in search of safer, more accessible tools.

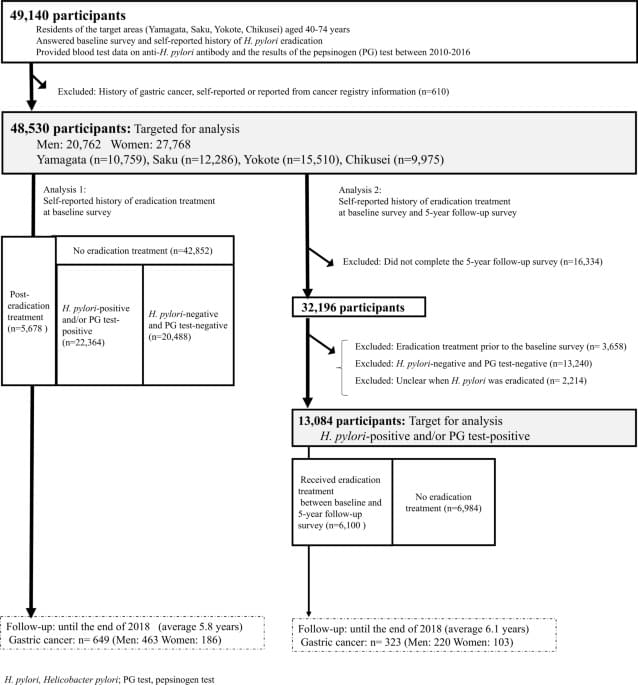
Helicobacter pylori (H. pylo ri) infection is an established cause of gastric cancer. Although H. pylo ri eradication is suggested to decrease gastric cancer risk, this has not been fully investigated in general populations. This analysis included 48,530 Japanese men and women aged 40–74 years from four cohort studies. At baseline, the participants provided a self-reported eradication history and serum anti–H. pylo ri IgG titers and the results of a pepsinogen (PG) test. We examined the association between eradication history and gastric cancer risk considering H. pylo ri positivity and PG testing using Cox proportional hazards regression models. From 2010 to 2,018,649 gastric cancer cases were diagnosed. Compared with those who were negative for both H. pylo ri and PG test as a reference, gastric cancer risk was 5.89 times higher (95%CI: 4.41–7.87) in those who were H. pylo ri-positive and/or PG test-positive and with no eradication at baseline. Gastric cancer risk among those who underwent eradication before baseline decreased after a temporal increase in risk following eradication (baseline to 1y: HR 1.74, 95%CI 1.18–2.57; 1y to Ono, A., Tanaka, S., Sawada, N. et al. Sci Rep 15, 21,307 (2025). https://doi.org/10.1038/s41598-025-00713-z.