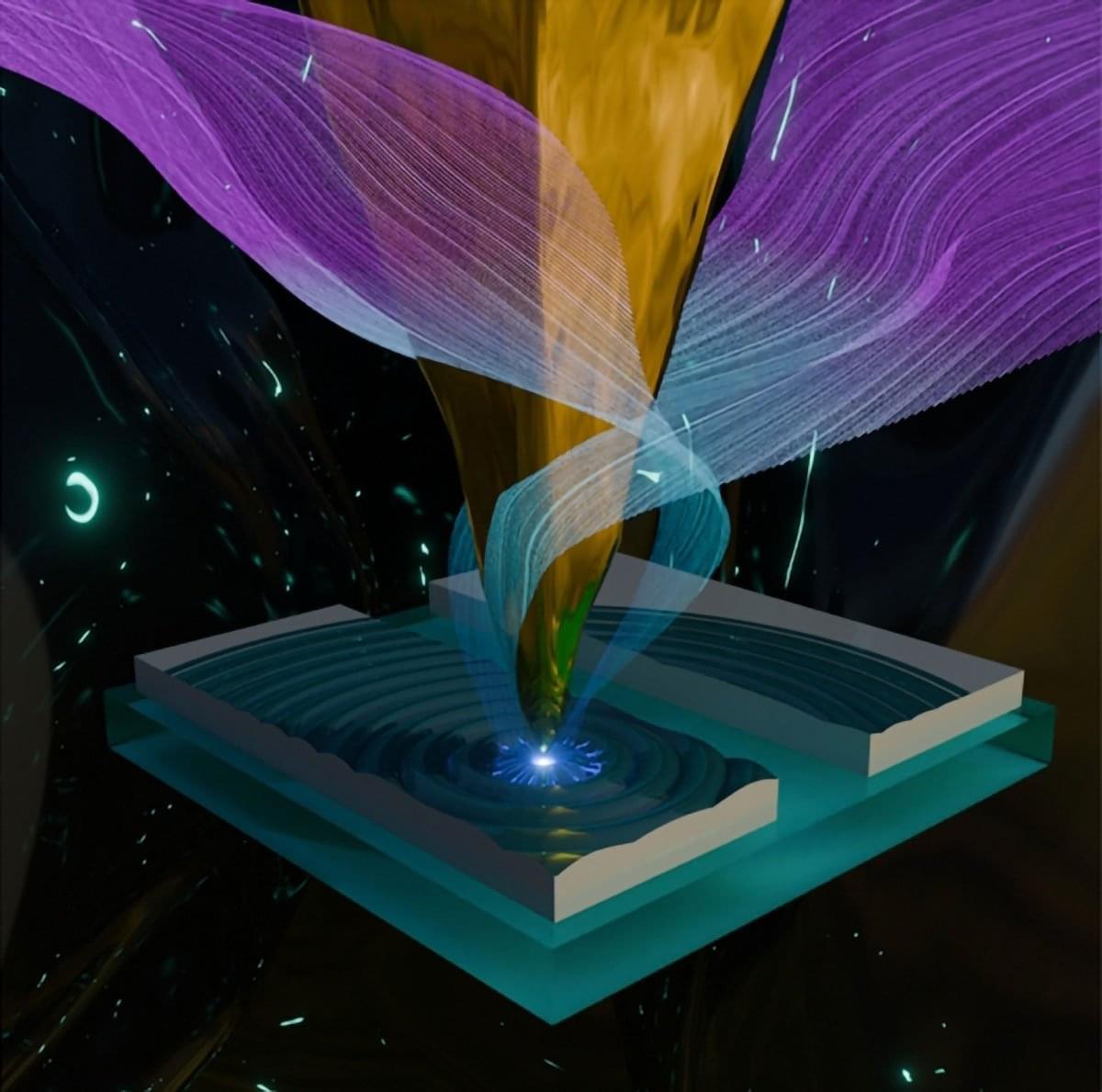
Zap Energy has advanced its Century fusion engineering test platform to operate for more than one hundred plasma shots at 0.2 Hz, or one shot every five seconds, with the resulting heat captured by surfaces coated with circulating liquid metal.
Concentrated inside a vacuum chamber about the size of a hot water heater, each plasma carried up to 500 kA of current—about 20 times stronger than a bolt of lightning—discharged into a vessel lined with flowing liquid bismuth. During the record run, Century’s total input power was 57 kilowatts, with 39 kilowatts delivered directly to the cables leading to the plasma chamber.
Compared with Century’s commissioning milestone in 2024, this achievement represents an increase of 20 times in sustained average power and is a major step toward developing commercial fusion power plants using repetitive pulsed power and liquid metal energy transfer.