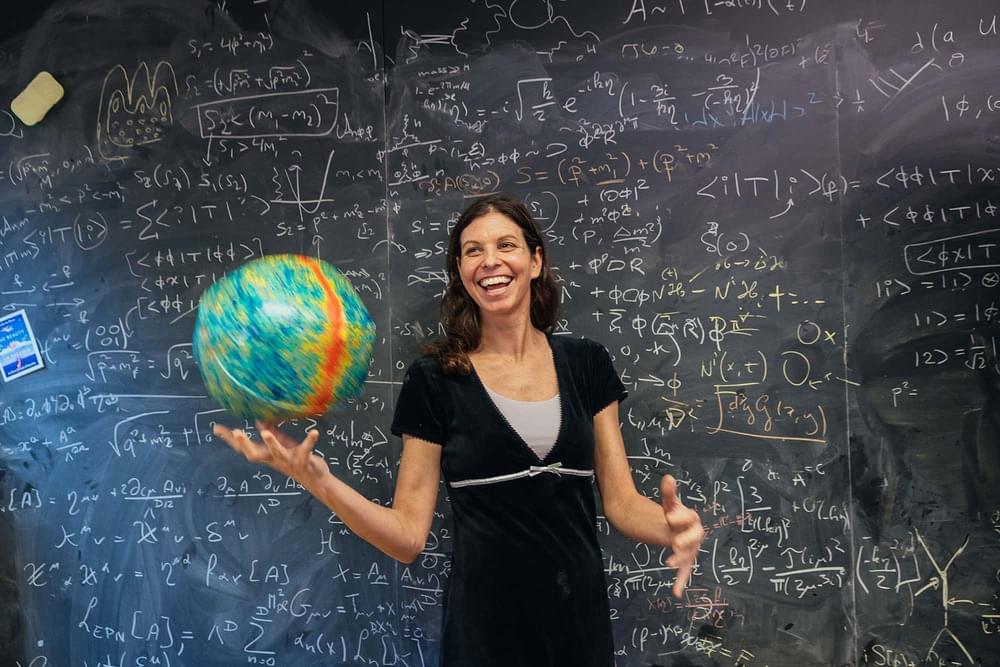
A very relevant subject for research.
The world appears to contain diverse kinds of objects and systems—planets, tornadoes, trees, ant colonies, and human persons, to name but a few—characterized by distinctive features and behaviors. This casual impression is deepened by the success of the special sciences, with their distinctive taxonomies and laws characterizing astronomical, meteorological, chemical, botanical, biological, and psychological processes, among others. But there’s a twist, for part of the success of the special sciences reflects an effective consensus that the features of the composed entities they treat do not “float free” of features and configurations of their components, but are rather in some way(s) dependent on them.
Consider, for example, a tornado. At any moment, a tornado depends for its existence on dust and debris, and ultimately on whatever micro-entities compose it; and its properties and behaviors likewise depend, one way or another, on the properties and interacting behaviors of its fundamental components. Yet the tornado’s identity does not depend on any specific composing micro-entity or configuration, and its features and behaviors appear to differ in kind from those of its most basic constituents, as is reflected in the fact that one can have a rather good understanding of how tornadoes work while being entirely ignorant of particle physics.