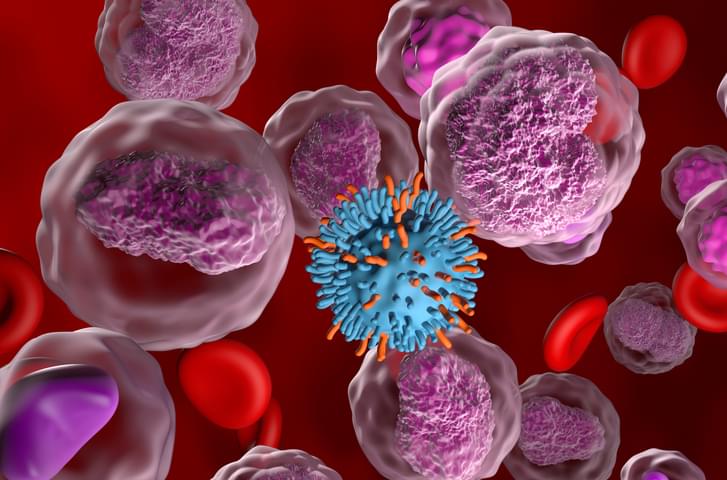
(Philadelphia, PA) – A single injection of a novel CRISPR gene-editing treatment safely and efficiently removes SIV – a virus related to the AIDS-causing agent HIV – from the genomes of non-human primates, scientists at the Lewis Katz School of Medicine at Temple University now report. The groundbreaking work complements previous experiments as the basis for the first-ever clinical trial of an HIV gene-editing technology in human patients, which was authorized by the Food and Drug Administration (FDA) in 2022.
The preclinical study, published online in the journal Gene Therapy, tested EBT-001, an SIV-specific CRISPR-Cas9 gene-editing therapy, in rhesus macaques. The study shows that EBT-001 effectively excises SIV from reservoirs – cells and tissues where viruses like SIV and HIV integrate into host DNA and hide for years – without any detectable off-target effects in animals. The work is a significant advance in the generation of a cure for HIV/AIDS in humans.
“Our study supports safety and demonstrates evidence of in vivo SIV editing of a CRISPR gene-editing technology aimed at the permanent inactivation of virus in a broad range of tissues in a large, preclinical animal model, using a one-time injection of the treatment,” said Kamel Khalili, PhD, Laura H. Carnell Professor and Chair of the Department of Microbiology, Immunology, and Inflammation, Director of the Center for Neurovirology and Gene Editing, Director of the Comprehensive NeuroAIDS Center at the Lewis Katz School of Medicine, and senior investigator on the new study.