The identification of a new type of symmetry in statistical mechanics could help scientists derive and interpret fundamental relationships in this branch of physics.
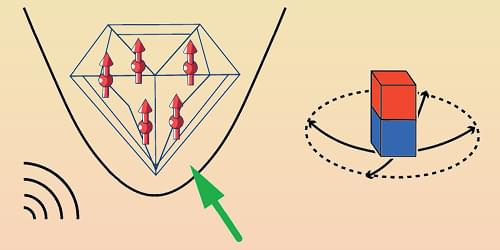
Symmetry is a foundational concept in physics, describing properties that remain unchanged under transformations such as rotation and translation. Recognizing these invariances, whether intuitively or through complex mathematics, has been pivotal in developing classical mechanics, the theory of relativity, and quantum mechanics. For example, the celebrated standard model of particle physics is built on such symmetry principles. Now Matthias Schmidt and colleagues at the University of Bayreuth, Germany, have identified a new type of invariance in statistical mechanics (the theoretical framework that connects the collective behavior of particles to their microscopic interactions) [1]. With this discovery, the researchers offer a unifying perspective on subtle relationships between observable properties and provide a general approach for deriving new relations.
The concept of conserved, or time-invariant, properties has roots in ancient philosophy and was crucial to the rise of modern science in the 17th century. Energy conservation became a cornerstone of thermodynamics in the 19th century, when engineers uncovered the link between heat and work. Another important type of invariance is Galilean invariance, which states that the laws of physics are identical in all reference frames moving at a constant velocity relative to each other, resulting in specific relations between positions and velocities in different frames. Its extension, Lorentz invariance, posits that the speed of light is independent of the reference frame. Einstein’s special relativity is based on Lorentz invariance, while his general relativity broadens the idea to all coordinate transformations. These final examples illustrate that invariance not only provides relations between physical observables but can shape our understanding of space, time, and other basic concepts.