Take a look at this excellent article that addresses the fundamental inability of science to solve the hard problem of consciousness:
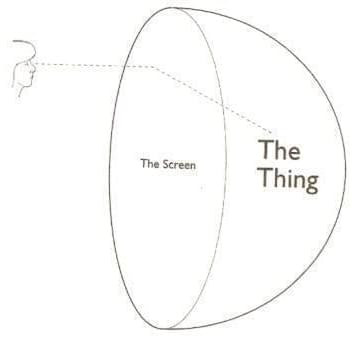
Imagine a scale that ranks civilizations not by their borders or technology, but by the sheer energy they command— some spanning entire galaxies. Join us as we explore the Kardashev Scale, the ultimate measure of cosmic power.
Watch my exclusive video Big Alien Theory https://nebula.tv/videos/isaacarthur–… Nebula using my link for 40% off an annual subscription: https://go.nebula.tv/isaacarthur Get a Lifetime Membership to Nebula for only $300: https://go.nebula.tv/lifetime?ref=isa… Use the link gift.nebula.tv/isaacarthur to give a year of Nebula to a friend for just $30. Visit our Website: http://www.isaacarthur.net Join Nebula: https://go.nebula.tv/isaacarthur Support us on Patreon: / isaacarthur Support us on Subscribestar: https://www.subscribestar.com/isaac-a… Facebook Group:
/ 1,583,992,725,237,264 Reddit:
/ isaacarthur Twitter:
/ isaac_a_arthur on Twitter and RT our future content. SFIA Discord Server:
/ discord Credits: The Kardashev Scale & Population Episode 486; February 13, 2025 Written, Produced & Narrated by: Isaac Arthur Editors: Ludwig Luska Graphics: Fishy Tree, Jeremy Jozwik, Ken York YD Visual Select imagery/video supplied by Getty Images Music Courtesy of Epidemic Sound http://epidemicsound.com/creator Phase Shift, “Forest Night” Chris Zabriskie, “Unfoldment, Revealment”, “A New Day in a New Sector”, “Oxygen Garden” Stellardrone, “Red Giant”, “Billions and Billions“
Get Nebula using my link for 40% off an annual subscription: https://go.nebula.tv/isaacarthur.
Get a Lifetime Membership to Nebula for only $300: https://go.nebula.tv/lifetime?ref=isa…
Use the link gift.nebula.tv/isaacarthur to give a year of Nebula to a friend for just $30.
Visit our Website: http://www.isaacarthur.net.
Join Nebula: https://go.nebula.tv/isaacarthur.
Support us on Patreon: / isaacarthur.
Support us on Subscribestar: https://www.subscribestar.com/isaac-a…
Facebook Group: / 1583992725237264
Reddit: / isaacarthur.
Twitter: / isaac_a_arthur on Twitter and RT our future content.
SFIA Discord Server: / discord.
Credits:
The Kardashev Scale & Population.
Episode 486; February 13, 2025
Written, Produced & Narrated by: Isaac Arthur.
Editors: Ludwig Luska.
Graphics: Fishy Tree, Jeremy Jozwik, Ken York YD Visual.
Select imagery/video supplied by Getty Images.
Music Courtesy of Epidemic Sound http://epidemicsound.com/creator.
Phase Shift, \

On this episode of Cultivate Curiosity, our host Jacie takes us on a journey through a few spectacular upcoming astronomical events. From February’s dazzling planetary alignments and bright Venusian glow to March and April’s upcoming eclipses and meteor showers, we explore the science behind these celestial events and how to best view them. Whether you’re an avid stargazer or just looking up with curiosity, this episode will inspire you to keep your eyes on the sky!
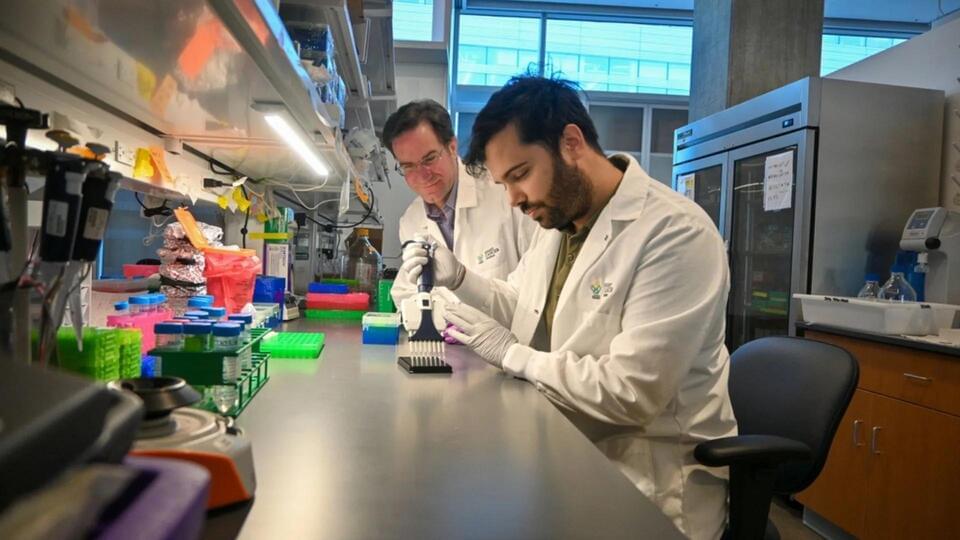
A new blood test developed by researchers at Oregon Health & Science University (OHSU) shows promise for the early detection of pancreatic cancer, a disease notorious for its high mortality rates due to late diagnosis.
The test, named PAC-MANN, which stands for “protease activity-based assay using a magnetic nanosensor,” could provide a critical tool for doctors.
It can potentially lead to improved survival rates for patients diagnosed with pancreatic ductal adenocarcinoma (PDAC), the most prevalent and aggressive form of pancreatic cancer.
Aging is a natural process, but for centuries, humans have been searching for ways to slow it down or even reverse it. Recent advancements in stem cell research and regenerative medicine have given scientists unprecedented insights into aging and potential interventions. With breakthroughs in cellular therapy, gene editing, and tissue engineering, we are closer than ever to finding ways to rejuvenate the human body. But how close are we to reversing aging, and what challenges remain?
Stem cells are the body’s raw materials from which all other specialized cells are generated. They have the unique ability to divide and create identical copies of themselves (self-renewal) or differentiate into specialized cell types. However, as we age, our stem cells decline in both number and efficiency, contributing to tissue degeneration, slower healing, and an increased risk of age-related diseases.
Researchers have been investigating how stem cells can be manipulated to repair damaged tissues, regenerate organs, and potentially reverse signs of aging. By harnessing stem cells, scientists aim to restore youthful function in various tissues and organs, offering promising anti-aging therapies.
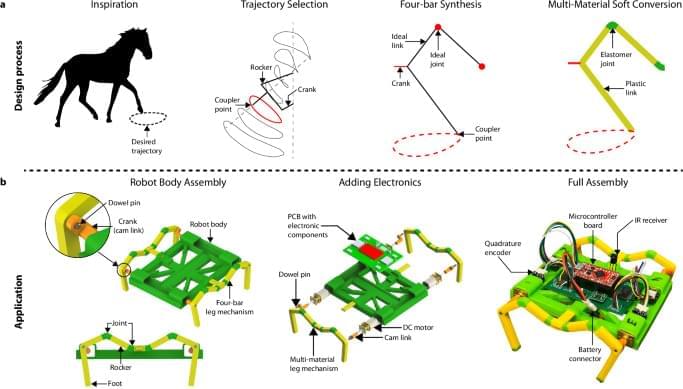
Soft robots excel in safety and adaptability, yet their lack of structural integrity and dependency on open-curve movement paths restrict their dexterity. Conventional robots, albeit faster due to sturdy locomotion mechanisms, are typically less robust to physical impact. We introduce a multi-material design and printing framework that extends classical mechanism design to soft robotics, synergizing the strengths of soft and rigid materials while mitigating their respective limitations. Using a tool-changer equipped with multiple extruders, we blend thermoplastics of varying Shore hardness into monolithic systems. Our strategy emulates joint-like structures through biomimicry to achieve terrestrial trajectory control while inheriting the resilience of soft robots. We demonstrate the framework by 3D printing a legged soft robotic system, comparing different mechanism syntheses and material combinations, along with their resulting movement patterns and speeds. The integration of electronics and encoders provides reliable closed-loop control for the robot, enabling its operation across various terrains including sand, soil, and rock environments. This cost-effective framework offers an approach for creating 3D-printed soft robots employable in real-world environments.
Soft mechanism driven robots, made via multi-material 3D printing, combine soft and rigid components for robust, adaptable locomotion. This framework balances flexibility and strength, enabling effective operation across varied terrains.
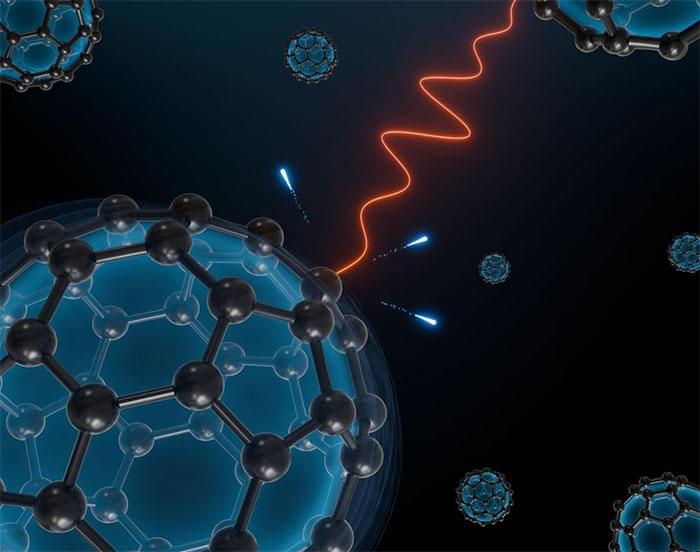
Light-sensitive nanoparticles promise a wide range of applications, for example in the field of sensor technology or energy generation. However, these require knowledge and control of the processes taking place within them. Plasmons, collective electron movements in the nanoparticle which transport energy, are essential in the behaviour of such nanoparticles.
Time-resolved experiments in the attosecond range reveal now that the importance of electronic correlations in these plasmons increases when the size of a system decreases to scales of less than one nanometre.
The study, published in the journal Science Advances (“Correlation-driven attosecond photoemission delay in the plasmonic excitation of C 60 fullerene”), was led by the University of Hamburg and DESY as part of a collaboration with Stanford, SLAC National Accelerator Laboratory, Ludwig-Maximilians-Universität München (LMU), Northwest Missouri State University, Politecnico di Milano and the Max Planck Institute for the Structure and Dynamics of Matter (MPSD).

Summary: New research provides direct evidence that the gut microbiome communicates with the brain through the vagus nerve. Using germ-free mice, scientists observed significantly reduced vagal nerve activity, which returned to normal after introducing gut bacteria.
When antibiotics were used to eliminate bacteria in normal mice, vagal activity dropped but was restored when microbiome-derived intestinal fluids were reintroduced. Specific metabolites, including short-chain fatty acids and bile acids, were identified as key activators of vagal neurons.
These signals extended to the brainstem, confirming a clear gut-to-brain pathway. The findings advance understanding of the gut-brain axis and may lead to new treatments for neurological and gastrointestinal disorders.