Northwestern University engineers have developed a pacemaker so tiny that it can fit inside the tip of a syringe — and be non-invasively injected into the body.
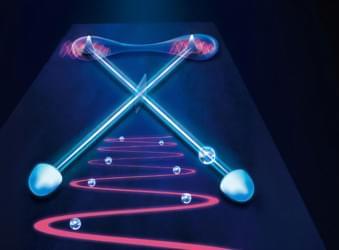
Smaller than a single grain of rice, the pacemaker is paired with a small, soft, flexible, wireless, wearable device that mounts onto a patient’s chest to control pacing. When the wearable device detects an irregular heartbeat, it automatically shines a light pulse to activate the pacemaker. These short pulses— which penetrate through the patient’s skin, breastbone and muscles — control the pacing. #Repost
Although it can work with hearts of all sizes, the pacemaker is particularly well-suited to the tiny, fragile hearts of newborn babies with congenital heart defects.
Designed for patients who only need temporary pacing, the pacemaker simply dissolves after it’s no longer needed. All the pacemaker’s components are biocompatible, so they naturally dissolve into the body’s biofluids, bypassing the need for surgical extraction.