In this interview, hosted by Nicolás Cherñavsky, Nir Barzilai and Brad Stanfield discuss metformin, whether or not to use it in non-diabetic patients to slow aging, and the TAME trial.
Nir Barzilai is president of the Academy of Health and Lifespan Research (https://www.ahlresearch.org/), and Brad Stanfield is a primary care physician in Auckland (New Zealand) and runs a YouTube channel (/ @drbradstanfield) with around 250,000 subscribers to explore the latest research and preventive care guidelines.
Host: Nicolás Cherñavsky.
Production: Nicolás Cherñavsky and Nina Torres Zanvettor.
Editing: Nina Torres Zanvettor.
Revision and subtitling: Nicolás Cherñavsky.
============================================================
Notes:
TAME trial website: https://www.afar.org/tame-trial.
Diabetes Prevention Program Outcomes Study (DPPOS): https://repository.niddk.nih.gov/stud…
UK metformin vs sulfonylurea trial on type 2 diabetics: https://www.cmajopen.ca/content/2/3/E162
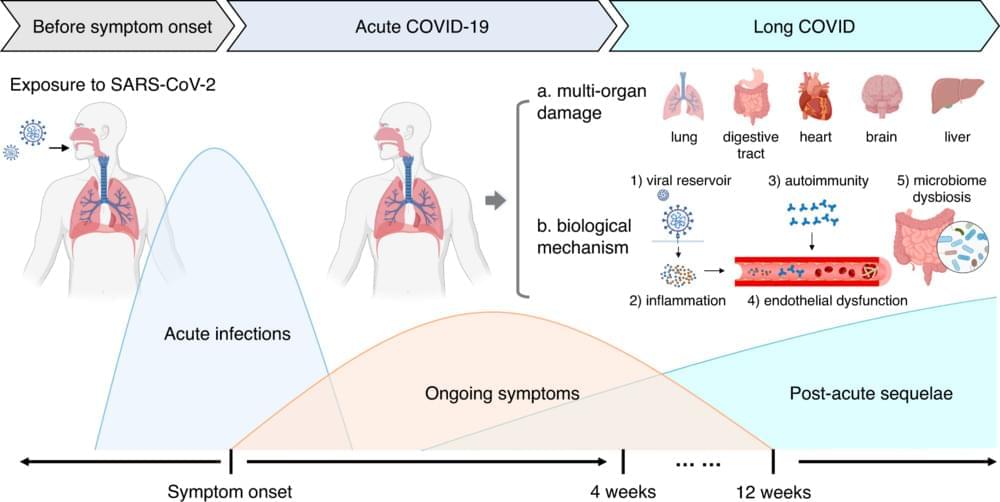
The New England Journal of Medicine paper on metformin treatment in Covid-19 patients: https://www.nejm.org/doi/full/10.1056…
Lancet paper on metformin treatment in Covid-19 patients: https://www.thelancet.com/journals/la…
Andre Scott’s paper on the cost-effectiveness of treating aging: https://www.nature.com/articles/s4358…
Medical guidelines database mentioned by Brad Stanfield: https://uptodate.com.
============================================================
Heales website (Healthy Life Extension Society): https://heales.org/
Contact e-mail: [email protected].